Annette T. Maruca1*, Deborah Shelton2 and William D. Barta3
1Sigma Theta Tau: Mu Chapter, University of Connecticut, School of Nursing, 231 Glenbrook Road, Storrs, CT 06269 USA
2Center for Correctional Health Networks–CCHNet, University of Connecticut, Storrs Hall,231 Glenbrook Road, Storrs, CT06269
3Center for Correctional Health Practice-Based Research Networks,University of Connecticut, Storrs Hall 231 Glenbrook Road, Storrs, CT 06269
Received: 15 April 2015 Accepted: 04 May 2015 Published: 11 May 2015
Visit for more related articles at Research & Reviews: Journal of Nursing and Health Sciences.
This pilot study examines the effectiveness of a 4-session booster treatment intervention for offenders with mental illness in a correctional setting prior to transition to the community. This was a quantitative self-controlled case series design study. The twenty consenting female offenders in a correctional setting were non-randomly assigned to four groups of five members. Three repeated measures of data collection using two surveys occurred at baseline, pretest and posttest. Data were analyzed using hierarchical linear modeling. This pilot study provides preliminary support for the effectiveness of a booster intervention in correctional institutions in bolstering and reinforcing previously learned self-care behaviors. Results revealed that the change in self-care behaviors observed was small yet potentially clinically meaningful. Not only did the booster intervention reinforce self-care behaviors, but also the brevity of the intervention supported treatment adherence. A booster intervention is clinical significant because it can maximize skills, reinforce knowledge, sustain treatment engagement and assist with transition to the community while supporting treatment completion.
Booster Intervention; Corrections; Offenders; Mental Illness; Mental Health Treatment.
Research shows that treatment interventions in correctional settings aimed at improving cognitive skills, problem solving, goal setting and stress management has a positive effect on reducing recidivism for offenders [1,2]. Research evidence further shows that cognitive-behavioral approaches to treatment were effective among offenders with high-risk behavior [3-5]. Despite the positive evidence on the efficacy of treatment interventions and particularly cognitive-behavioral approaches, treatment effects tend to gradually diminish over time [6].
A booster intervention may be effective in the correctional setting to address the concern of diminishing treatment effects. A booster intervention shortens an existing, effective treatment program to reinforce skills previously learned. Correctional settings offer unique challenges in the delivery of health care services, particularly for offenders who struggle with mental illness. Some challenges inherent to the correctional system include unanticipated early releases, transfers of offenders between facilities, or unit lock-downs that all interfere with offenders completing treatment programs. The correctional environment promotes dependency and adherence to rules. This type of culture can constrain self-care behaviors, with self-care defined as the practice of behaviors that protect and promote one’s health and wellbeing [7,8].
An evidence-informed cognitive behavioral treatment intervention has been developed and implemented in a state Department of Correction (DOC) to treat offenders with behavioral disorders. The modified cognitive behavioral program offers thirty-two sessions in four units: (1) basic foundational skills, (2) coping with emotions, (3), interpersonal skills, and (4) future focused skills. The configuration of the booster treatment intervention mirrors the four units of the primary 32-session program. The sessions are built upon cognitive-behavioral principles of changing thought patterns and the behaviors that result from these thought patterns, in order to alert the individual to the emotional reactions that can occur in response to situations. The primary investigator was trained to maintain conformity to the original program; to gain familiarity with the population of offenders with mental illness preparing for release.
The purpose of this pilot study was to investigate the effectiveness of a four session’s booster intervention in a New England’s prison that examined self-care behaviors and mental health status. The research question was “What is the effect of a booster treatment intervention on self-care behaviors and mental health status for offenders preparing for reentry?” The hypothesis was that participants would show improved self-care behaviors and maintenance in mental health symptoms after the booster treatment intervention. The assumption was that participants who received the booster treatment intervention would benefit from the booster intervention by reinforcing self-care behaviors and maintaining treatment gains learned during the primary program.
Offenders often lose their sense of autonomy and ability to practice self-care in the prison environment that constrains such practices. As the offender prepares for release back to the community, these abilities are fundamental to successful transitioning. The booster treatment intervention reintroduces and emphasizes the use of skills such as coping, assertive communication, interpersonal, and future planning that are important components of relearning and practicing self-care behaviors. The Rediscovery of Self-Care: A Care Model for Persons with Incarceration Experience model frames the research question to explore the effectiveness of the booster intervention designed to support reinforcing self-care behaviors and coping skills aimed to enhance the physical, mental, emotional and psychological health of offender’s as part of their community reentry [9]. This model offers a conceptual approach to assessing changes in released offender’s practice of self-care related to treatment intervention.
Design
This study employed a self-controlled case series design [10]. A key characteristic of this design is that participants serve as their own control so history effects are not a concern and all observations are categorized as either treatment a usual or intervention. Three data collection points included baseline (recruitment), pretest (beginning of intervention), and posttest (end of intervention). An advantage of the method is that confounding factors that do not vary with time, such as treatment as usual, is controlled for implicitly.
Recruitment, Sample Size and Informed Consent procedure
The twenty consenting participants were not randomized to groups, but selected based on meeting inclusion criteria (completed three or four units of the primary program, had a release date within one year, were 18 years of age or older, spoke English, and had mental health or substance abuse problems) and willingness to volunteer. Institutional Review Board approval (IRB Protocol #H12-314) from the University of Connecticut and from the state Department of Corrections (DOC) Research Advisory Committee was obtained prior to recruitment. There were four groups each with five members per group [11].
An appraisal of systematic reviews showed that a booster treatment intervention has not been implemented and tested in correctional institutions upon which to base the sample size for this pilot study [12-14]. However, studies on the effectiveness of interventions used for offenders with mental illness in correctional settings have shown to be cautiously effective with small to moderate effect sizes [12,15,16].
Procedures to protect participant confidentiality included: meeting in a private, but visible space; explanation of the purpose of the study, time requirements and expectations of the study; and, the voluntary nature of their participation. Any questions were answered and clarified as needed. Offenders who agreed to volunteer were asked to sign the consent form and to complete the demographic sheet along with the two surveys.
Data Collection
Demographic information was obtained using a self-report information sheet that was collected at the time of recruitment and included information such as age, level of education, ethnicity, and participation in other treatment groups.
Instruments
The Strategies Used by People to Promote Health (SUPPH) is a 29-item self-report scale developed to measure an individual’s confidence in their ability to accomplish self-care behaviors [17]. Refinement of the SUPPH, by Lev, Paul and Owen to validate the dimensionality of the measure supported a three-factor structure: positive attitude (Cronbach’s alpha = .92); stress (Cronbach’s alpha = .89); and making decisions (Cronbach’s alpha = .83) [18]. Mak et al’s study on social support as a mediator for self-care self-efficacy also achieved excellent internal consistencies for the SUPPH’s three subscales (Cronbach’s alphas = 0.95, 0.90, and 0.80 for positive attitude, stress and making decisions) [19]. Participants are asked to rate the degree of confidence they have in carrying out self-care behaviors as they experience re-entry issues on a scale from 1 (very little) to 5 (quite a lot). The higher the total score (range from 29 to 145) indicates higher confidence in self-care skills and the ability to perform self-care behaviors.
The SUPPH has been used to measure self-care behaviors with cancer patients [17], hemodialysis, and with depression [20-22]. This instrument had never been used with the correctional population and the reading level was not defined.
The Behavior and Symptom Identification Scale-24 (BASIS-24), is an outcome measure of self-reported psychological difficulty that has been used with inpatient and outpatient mental health populations. BASIS-24 measures general and mental health status, substance abuse, social and community functioning, and quality of life. Internal consistency reliability (Cronbach’s alpha) coefficients ranged from 0.75 to 0.89 for inpatients and 0.77 to 0.91 for outpatients [23]. Eisen et al’s (2006) study measured the reliability and validity for three race/ethnicity groups (White/African-American/Latino) with Cronbach’s alpha coefficients exceeding 0.70 for each ethnic group (p. 313) [24]. BASIS-24 contains 24 items, each with five ordered responses, reporting either the level of difficulty experienced (0 = no difficulty to extreme difficulty to 4 = extreme difficulty) or the frequency that a symptom has occurred (0 = none of the time to 4 = all of the time).
The 24 questions are scored using a weighted average algorithm that yields six subscales and an overall score. The lower the total overall score out of a total possible score of 96, the less difficulty the respondent self-reports on mental health symptoms (lower score = better mental health status). One question pertaining to “hiding drugs or alcohol” was removed following IRB reviews and at IRB bidding with permission from McLean hospital. Questions are at a fifth grade reading level, are brief, and are easily understood. BASIS-24 was used with a corrections population (parolees) to measure the effectiveness of the primary program with this population.
Intervention
The focus of intervention was to: (a) improve self-control of impulses, (b) recognize social and emotional cues, (c) regulate emotional responses to cues, (d) improve decision making based on consequences, and (e) improve use of coping strategies and stress management with the desired outcome of enhanced self-care behaviors. Participants were provided individual worksheets in a DOC approved folder to keep for reference and as part of homework assignments. A Certificate of Completion was given to participants at the end of the intervention if participants completed all sessions.
Data Analysis
Descriptive statistics were performed using SPSS version 16.0 to provide descriptive sample summaries such as mean age, average educational level, distribution of ethnicity and the number of primary program units completed. Data analysis was performed using Hierarchical Linear Model 7.01 student version statistical program (HLM), also referred to as random coefficient model, mixed model or multilevel model [25]. When comparing scores on the same measure collected from the same person on several occasions, it is expected that scores will be highly correlated. With HLM, independence was not required because it was violated at each level of the analysis and reduced the likelihood of a type I error.
HLM piecewise growth model examined within individual differences (Level 1) as well as modeled intercepts and slopes as a function of between individual differences (Level 2). A piecewise growth model can estimate growth trajectories measured within and across individuals and account for variation in the self-care (SCVAR) and mental health (MHVAR) outcomes. This type of modeling can demonstrate if there is a trend in score over time, if groups have an effect on the trend, and if there is a pattern to the change indicating a relationship between these variables [26]. Unlike the traditional repeated measures analysis of variance (ANOVA), HLM does not delete cases from the analysis because of missing time points, therefore, does not reduce sample size [27].
Level 1Predictors
The Level-1 predictor variables for time were used to capture repeated measures over time for treatment as usual (TAU) and intervention (INTV) with the three time points recoded into two dummy variables [28]. A code for time = 1 is baseline, for time =2 is pretest, and for time = 3 is posttest. The first time segment for treatment as usual represents the linear growth during baseline to pre-test time segment. The second time segment for the intervention represents the growth slope of the booster intervention. When time is coded in this way, the parameter captures how much between-person variability exists in terms of where each person starts. Each time segment indicates the correlation between individuals’ initial scores (intercepts) and their growth rates (slopes). The time variable, predictors of the self-care outcome variable, designates “the within-person structure can be both heteroscedastic and correlated over time” [29].
Level 2 Predictors
The level-2 predictor variables contained information about compositional and contextual factors. Age, education, and group membership were removed because they did not contribute to the model and had non-significant effects as predictors for either self-care (SC) outcomes or mental health (MH) status. The number of individuals in each group who completed four units of the primary program (FOURS) and the number of individuals in each group with severe degree of self-reported difficulty with mental health symptoms (SEV_MH) both significantly influenced self-care behaviors measures, therefore, were retained as level 2 predictors. Baseline and pretest scores for self-care and mental health were also retained as level 2 predictors.
The mental health subscale for self-harm in the BASIS-24 instrument consisted of only two items, question 11 (“think of ending your life”) and question 20 (“think about hurting yourself”). Scores showed 90% (18 out of 20) of the participants had scores for self-harm equal to zero indicating “no difficulty with self-harm thoughts”. Based on a review of the literature concerning the prevalence of self-harm behaviors in prison and on a discussion among the research team that near to release offenders will withhold feelings of self-harm because it may interfere with their release date, the decision was made not to retain the self-harm subscale in the mental health variable.
Centering of variables was based on the researcher’s interest in the individual’s performance and the recognition that group effects can impact the results or be a “nuisance factor”. Centering can improve the interpretability of the coefficients and reduce multicollinearity [24]. Grand mean centering reduces correlation across groups and reflects the group average. If the value of zero for a predictor is not meaningful, the intercept will lack meaningful interpretation and the estimate may lack precision. When these conditions exist, centering is advisable [30].
After data were entered, the first step to creating the HLM model was the null model using self-care as the outcome measure (SCVAR) with no covariates to assess the degree of between group variance (Garson, 2014). The null model is similar to random effects ANOVA. The intercept was significant (p < 0.001) and the Intra-Class Correlation coefficient (ICC) was 0.70322 suggesting that about 70% of the variance in self-care scores can be explained by the differences between groups. The result of this unconditional model follows:
Final estimation of variance components
| Random Effect | Standard Deviation | Variance Component | d.f. | χ2 | p-value |
|---|---|---|---|---|---|
| INTRCPT1, u0 | 17.67177 | 312.29152 | 19 | 154.09196 | <0.001 |
| level-1, r | 11.47897 | 131.76667 |
The Final Model
Level 1 data were repeated observations obtained at three time points for each participant predicted as two time segments for treatment as usual (Time 1_TAU) and the booster intervention (Time 2_INTV). Both time segments, when added to the null model as predictor variables, were significant at the p < 0.05 statistical level. Level 2 data consisted of compositional and contextual factors. These included baseline scores (MHT1, SCT1), pretest scores (MHT2, SCT2), number of completed SN units (FOURS) and severity of self-reported mental health difficulties (SEV_MH). The institutional level was not considered as a level of statistical analysis since all female offenders reside in one state correctional institution. The limited sample size did not allow for a three-level model to be analyzed. When mental health was the outcome variable, individual’s self-care was not significant for treatment as usual (b = 0.09, SD = 0.12, t = 0.72, df = 36, p = 0.478) or for the intervention (b = -0.13, SD = 0.07, t = -1.83, df = 36, p = 0.074) in predicting change in mental health status, so self-care was kept as the explanatory variable for the final model.
The resultant HLM 2 fixed effects model with self-care as the outcome variable is shown below:
Level-1 Model
SCVARti = π0i + π1i*(Time 1ti) + π2i*(Time 2ti) + eti
Level-2 Model
π0i = β00 + β01*(FOURSi) + β02*(SEV_MHi) + r0i
π1i = β10 + β11*(MHT1i) + β12*(SCT1i)
π2i = β20 + β21*(MHT2i) + β22*(SCT2i)
Demographics
Descriptive statistics provided the following summary of the sample. All participants were females with a mean age of 37.5 years. The sample ethnicity consisted of 20% Black (n=4), 65% Caucasian (n=13), 10% Latino/Hispanic (n=2), and 5% of Mixed ethnicity (n=1). In terms of education, 5% completed college, 21% completed high school and 42% completed one to two years of college while 16% had less than three years of high school and 16% had earned a GED. Most of the participants were single (55%) or were married (25%) while 5% were divorced, 10% were separated and 5% had significant others. A total of 40% of the participants completed all the primary program units while 60% had completed three primary program units.
Hypothesis Testing
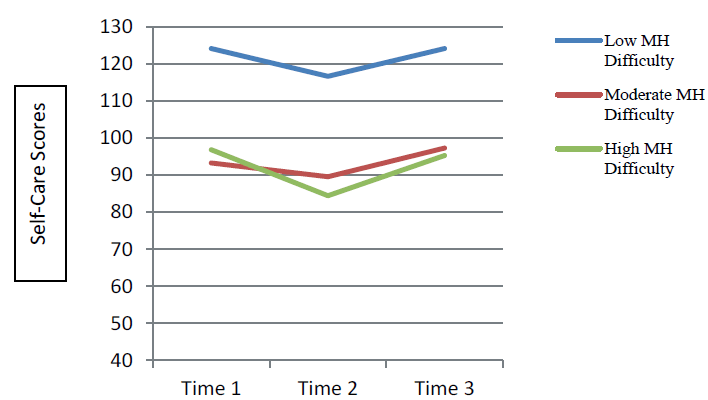
The research question was: “What is the effect of a booster treatment intervention on self-care behaviors and mental health status for offenders preparing for community reentry?” As was hypothesized, the booster intervention significantly influenced self-care behaviors showing an improvement after the booster (b = 8.75, SD = 3.15, t = 2.76, df = 34, p = 0.009) intervention (Table 1). There was a diminished treatment effect on self-care behaviors and on the status of mental health during treatment as usual (TAU). Self-care scores across individuals declined by 0.34 points from time 1 (baseline) to time 2 (pretest) and then improved after the intervention by 0.34 from time 2 (pretest) to time 3 (posttest). The same pattern was evident with mental health status that declined by 8.59 points from time 1 (baseline) to time 2 (pretest) and improved after the intervention by 6.82 points from time 2 (pretest) to time 3 (posttest). Interpretation of this result can be tenuous, as many factors may have influenced the outcome.
Results of across group analysis: Self-Care (dependent variable)
Treatment regression during TAU may have been influenced by the research design that employed a two-week wait period before beginning the intervention so participants can serve as their own control. The initial contact with the primary investigator during recruitment was followed by a noticeable absence of both the investigator and the intervention for two weeks during which time individuals returned to their routine. Another factor that influences research in correctional settings and effects treatment regression was the frequency of a facility lockdown where the group session could not be held. These lockdowns interrupted the sequential flow of group sessions and had an observable effect on group performance and dynamic.
Opposite to what was expected, individual’s self-care was not significant in predicting a change in mental health status both during treatment as usual (b = 0.09, SD = 0.12, t = 0.72, df = 36, p = 0.478) and the booster intervention (b = -0.13, SD = 0.07, t = -1.84, df = 36,p = 0.074). The marginal finding for the intervention period may be an artifact of the booster’s effect upon individuals. According to Heiman, volunteers for studies tend to exhibit an increased need for approval, and have a tendency to be less authoritarian and more conforming [31]. Also, those who participate and find the topic particularly interesting are more likely to evaluate the study on a positive level. Individuals who reported high difficulty with mental health symptoms also had lower confidence in self-care behaviors and those with low mental health difficulties reported higher self-care behaviors. However, regardless of the degree of perceived mental health difficulty, self-care behaviors for all groups (low, moderate and high) declined during TAU and then improved after the booster intervention.
In this pilot study, too few (2 out of 20) participants self-reported any difficulty with self-harm thoughts; therefore, any inferences about the self-harm would be inconclusive. According to the correctional literature there are disparate estimates on the prevalence of self-harm behaviors in prison [32,33]. Self-harm behaviors were estimated between 2% to 4% for offenders in the general population, while offenders with mental health disorders, had estimates of 15% self-harm behaviors. Department of Justice (DOJ) researchers found that 12% of female offenders self-reported self-harm behaviors [20]. This pilot study had similar results to these national estimates with 10% of female offender participants who self-reported self-harm behaviors in this sample.
In the absence of any previous study on boosters in correctional settings, a moderate effect size of the booster was anticipated based on the literature of booster interventions examined in educational and psychological literature. Since participants had prior exposure to these skills, it was expected that they would demonstrate more consistency, more proficiency and greater confidence in using self-care behaviors and coping skills in day-to-day activities and interactions. Using Raudenbush & Bryke’s (2002) concept of effect size as the “percent of variance explained” in the Level-2 model (r2 = [τ2null - τ2means]/τ2null), the booster intervention explains 25% of variance in self-care behaviors (p.47) [34].
This pilot study provides preliminary support for the effectiveness of a booster intervention in correctional institutions for reinforcing self-care behaviors. This is the first examination of a booster treatment intervention with a correctional population noted in the literature. The overall effects of correctional treatment and rehabilitation programs tend to be small to modest based on the evidence and this was evident in this pilot study as well [35-37]. The positive change in self-care behaviors observed was small yet potentially clinically meaningful.
Not only did the booster intervention enhance self-care behaviors, but it also supported adherence to the intervention. Offenders with mental illness may not comply with treatment resulting in limited treatment effectiveness. Based on participant attendance and comments, the four sessions seemed to appeal to participants [13,38]. It may be useful to consider stabilization of mental health symptoms prior to engaging in a booster intervention to support compliance. Other accommodations such as offering the booster during evening hours so as not to interfere with offender’s existing treatment program, work schedule and visiting hours; and providing a location for the intervention was away from distracting events had a positive effect on the satisfactory comments offenders shared with the primary investigator and contributed to the lack of attrition.
This pilot study helps to identify ways in which the booster intervention can be improved. First, addressing some of the barriers encountered with implementing this pilot study. Access to the offender participants was allowed only through a clinician who acted as the primary investigators liaison and often proved to be difficult causing interference with the research design and long delays between recruitment. Direct access for recruitment would improve study outcomes. Institutional factors unique to the correctional setting such as lockdowns, room cancellations where the intervention would be held, late starting due to evening count, and escort status as a visitor nurse researcher all were factors that interrupted the research design. This led greater than the prescribed two-week break between recruitment and the booster intervention and lengthened the research timeline. These are important issues to address in future studies.
According to Morgan et al. significant treatment gains that begin during incarceration and that continue with treatment services provided in the community are more likely to improve recidivism. A future study would be testing this booster in the community in correctional halfway houses for offenders with mental illness who were just released from prison. The benefit would be to encourage continued involvement in treatment, review and strengthen self-care behaviors when needed the most and avert treatment regression. This also allows for practice of self-care skills as offenders are transitioning back home.
This study had several limitations. First, the sample size was small, which limited the complexity of the HLM model, specifically not being able to examine another level of dependency with all variables [10]. Age, education and group membership were not significant in influencing self-care that may relate to small sample size rather than lack of significance. Second, this study was done with a selected group of motivated offenders based on their involvement in the primary program who matched the inclusion criteria. Motivation may have played a role in level of participation and compliance. Third, the study lacked a true control group for comparison related to political and programmatic reasons. It is challenging to evaluate the effectiveness of a treatment intervention in correctional settings, as it is rare to have only one treatment in operation at a time. Participants were involved in treatment as usual and could not be blinded to the treatment and knew they would be receiving the intervention. Fourth, conversations within and between group participants that occurred during daily contact in the prison may have influenced the outcome. This is hard to manage in a prison where offenders live in close quarters and are constantly together and talking. Future studies would benefit from randomization into a control and intervention group. Fifth, the primary researcher made every attempt to adhere to treatment protocol from training, yet skills do improve with experience and may impact the outcome. Also responses during interactions occur in context and are natural human interactions that can be a limitation. How individuals and groups interact with the primary researcher can affect different outcomes. Finally, there are few instruments specific to correctional settings. The surveys used were another limitation in this study because these surveys had not been tested in the correctional setting. Questions need to be applicable to life in prison to accurately measure the desired outcome. Also relying entirely on offenders self-report of change that occurred during each phase of the study is a limitation. Surveys are very prone to contain volunteer bias. Those who are willing to volunteer tend to have a particular attitude or characteristics (e.g., motivation) versus those who are not willing to participate (e.g., bored) [11]. The more motivated participants are the better their responses to the questions to satisfy the investigator. Future studies would want to modify questionnaires and then test these instruments for validity and reliability with the corrections population.
Despite the limitations of this pilot study, results do indicate that a booster intervention for offenders with mental illness in the prison setting can be significant for enhancing learned behaviors, practicing new skills and promoting treatment adherence. It is important to apply evidence-based correctional treatment programing to offenders with mental illness and evaluate the effectiveness. The significance of this research study is its exploration of a booster program uniquely situated within the correctional system to bolster the reentry process for offenders. One benefit of a booster intervention, as seen from this study is compliance to treatment interventions. The brevity of the intervention and treatment characteristics previously mentioned were positive elements of the booster. In conclusion, this supports further development and testing of the use of booster interventions in this setting.
This manuscript is part of the first author’s dissertation research and she would like to express special thanks to Dr. Shelton, her major Advisor. Dr. Shelton selflessly shared her knowledge and expertise as a nurse researcher, correctional nurse expert and academician. Dr. Barta offered his knowledge and expertise in data analysis and was vital in the first author’s understanding of HLM.