ISSN: 2322-0066
ISSN: 2322-0066
Kibreab Tesfamicael Haile1, Meron Berhe Tsegai1*, Feven Niguse Sielu1, Liya Tekle Weldu1, Tesfit Brhane Nesserab2, Eyasu Habte Tesfamariam3
1Department of Health Science, Asmara University, Asmara, Eritrea
2Department of Physiology, Orotta College of Medicine and Health Sciences, Asmara, Eritrea
3Department of Statistics, Biostatistics and Epidemiology, Collage of Science, Eritrean Institute of Technology, Mai-Nefhi, Eritrea
Received: 16-Aug-2022, Manuscript No. JOB-22-71909; Editor assigned: 18-Aug-2022, PreQC No. JOB-22-71909 (PQ); Reviewed: 01-Sep-2022, QC No. JOB-22-71909; Revised: 26-Dec-2022, Manuscript No. JOB-22-71909 (R); Published: 02-Jan-2022, DOI: 10.4172/2322-0066.11.1.001
Visit for more related articles at Research & Reviews: Research Journal of Biology
Background: Even though dengue fever suspicion started to surface in the high altitude localities of Zoba Maekel, presence of the vector has not been studied. Therefore, the study aimed to identify the availability of Aedes mosquitoes, their breeding preferences, and level of infestation in fifteen localities of this region.
Methods: Inspection of all water holding containers, in 740 systematically selected households of fifteen localities, was done identifying immature stages of Aedes mosquitoes. All immatures were then, classified, reared and identified using taxonomic keys. Breeding preferences ratio and infestation indices were calculated.
Results: In this study Aedes Aegypti mosquito was found in four localities, whereas mosquito of other Aedes specie was identified in twelve localities. Out of all the households inspected 51 were positive for Aedes immature. All indoor containers studied were free of Aedes infestation, whilst 53 of 874 outdoor containers were infested by Aedes larvae and pupae. In this study, discarded tyres were found to have the highest breeding preference ratio (2.11) and pupal productivity (40%). Plastic barrels had the highest positivity (42%) and were the second most productive type of container (28%). The household, container and breteau Indices of more than half of the localities were higher than the high transmission risk thresholds.
Conclusion: The study indicated possibilities of local dengue fever transmission in the studied areas. Hence, in depth confirmative studies should be considered and strategic preventive actions should be commenced in regard to the most preferred sites such as discarded tyres.
Dengue fever; Aedes aigypti; Aedes specie; High altitude; Mosquito breeding
BI: Breteau Index; BPR: Breeding Preference Ratio; CDC: Communicable Disease Control; CI: Container Index; DEN: Dengue; DHF: Dengue Haemorrhagic Fever; DSS: Dengue Shock Syndrome; EPLF: Eritrean People’s Liberation Front; GIS: Geographic information system; GPS: Global Positioning System; HI: House Index; HMIS: Health Management and Information System; IPCC: Intergovernmental Panel on Climate Change; IDSR: Integrated Disease Surveillance and Response; ASL: Above Sea Level; MoH: Ministry of Health; SPSS: Statistical Package for Social Science; WHO: World Health Organization
Dengue fever is a mosquito born viral disease that has grown to affect over half of the world’s population in the last 60 years. Globally, it is estimated to cause 390 million cases annually in 128 endemic countries, among which, 96 million cases are manifested clinically [1]. Besides, around 20,000 deaths are attributed per year to the sever version of the disease, in addition to 364 disability adjusted life years per million population per year, which are lost by its cause. The most seriously affected areas around the world include, Africa, American Eastern Mediterranean, South East Asia and Western Pacific regions [2]. Even though its occurrence in these areas may be affected by local spatial variations of rainfall, temperature, relative humidity, degree of unplanned urbanization and quality of vector control services in urban areas, its spread is expected to raise in response to climate change [3]. Concomitantly, the disease had presented itself for the first time in France and Croatia as of 2010, and is generally projected to emerge in Europe, high altitude regions of Eastern Africa and the Northern Andes, US and Canada [4,5].
The causative dengue virus (DEN) encompasses four serotypes belonging to the Flavivirus genus of the Flaviviridae family [6]. Isolation of at least one of these four serotypes by serology or by molecular diagnostic methods confirms dengue fever infection. Currently, even though several diagnostic kits are available in the market, one of the main diagnostic challenge remains to be absence of sensitive and specific diagnostic kits that are affordable and can diagnose the infection at an early stage [7].
The disease is carried and spread by the aid of several species of female Aedes genus mosquitoes, which prefer to bread in man made containers in a residential urban setting [8]. Mostly, transmission by this vector is favoured by temperature ranging between 14°C and 18°C, at the lower end, and 35°C and 40°C, at the upper end. The Ae. Aegypti or the African tiger mosquito is the primary vector and the specie with the highest transmission potential. Ae. Albopictos also known as the Asian tiger mosquito, likewise, has the potential to spread the disease and is recognized as the secondary dengue vector. As a result of its high adaptation to cooler temperatures, hibernation, and ability to shelter in microhabitats, this specie of Aedes mosquito had spread to North America and 25 countries in the European region from its ordinary territory in Asia. Generally, the vector is characterized by the silvery white patterned scaled body and, black and white striped legs [9]. Its distinct daytime feeding habit and peri domestic breading site preference are among its unique characteristics. This makes control efforts more difficult in addition to its almost imperceptible bites which, if needed, could take place upon several people at the same blood meal. This vector is mainly found in the tropical and subtropical regions of the world, where higher temperature during its immature stage favours adult mosquito’s dengue virus infection and transmission abilities. At adult stage, this temperate condition shortens incubation period of DENV, resulting in to lengthened transmission time of the mosquito, and increased biting frequency due to dehydration. Even though that’s the case, with the upcoming of urbanization, high rate of population growth, international travels, and climate change; it had the chance to spread globally [10-15].
In Africa, occurrence of dengue fever has been known since the mid 1920’s. Even though confirmatory laboratory tests are still lacked and surveillance data remains to be poor, dengue fever outbreaks and epidemics are reported from all regions of Africa. This being the case, results from published reports indicate most epidemics to occur in the Eastern region of Africa, followed by smaller scale epidemics in West Africa. Consequently, dengue fever endemicity is attested in 34 African countries by all 4 dengue fever virus serotypes, buttressed by the availability of Ae. Aegypti in all but five countries in the continent. Such attributes were influential in spreading the disease in the continent resulting in 16% of the overall infections globally as of 2010. This was the highest occurrence of the disease next to Southeast Asia, which contributed up to 70% of the infections at that time [16].
In Eritrea, the disease was first seen in 1990, after the liberation of the portal city Massawa from the Ethiopian colonization. During that time, almost all fighters of the Eritrean People’s Liberation Front (EPLF) contracted the disease and it was named “welcome” by the locals as sign of gratitude for the fighters. After that, the first confirmed outbreak was documented in 2005. Since 2010, the national HMIS/IDSR data indicates an overall increase in suspected dengue fever cases in Eritrea. Even though, dengue fever has shown an increasing pattern over the years, under-reporting due to possible miss diagnosis overlapping with malaria or other febrile illnesses could have affected it [17].
In Zoba Maekel, a region with altitude averaging about 2,250 m Above Sea Level (ASL), suspected dengue fever caseshave been reported in all subzones and presence of Ae. Aegypti mosquito has been confirmed in three villages by2018. This being the case, unavailability of laboratory or rapid diagnostic detection tools, limits the confirmation of allsuspected cases and in turn blocks identification of the diseases by its source. Hence, assessing presence of thevector mosquito in fifteen locations of this region can be helpful in assuring the possibility of dengue fevertransmission, and will be vital in tackling the possibly indigenous transmission in the areas. Results from this studycould also initiate in depth studies that can widen the current knowledge on the possibility of the disease’stransmission in these areas. For that reason, this study tries to identify the presence of dengue fever vectors in fifteenlocalities, and investigates the vectors preferable breeding sites and their levels of infestation [18].
Study area and study population
The study was done in ten villages of Zoba Maekel and five administrative areas of Asmara. All study sites are located in an area elevating from 2109–2349 m ASL. In the last 8 years, Asmara received average precipitation of 103.9 mm in Summer (June up to August) season, with intermittent rain in spring (March up to May) and Autumn (September up to November) averaging 32.6 and 15.9 mm correspondingly. At the same period, average minimum and maximum mean temperature in summer was 12.2 and 24.2oC, with average humidity of 71.4%. According to their respective local administrations, most of the localities get water from wells, drills or ponds; while, residents of the five administrative areas of Asmara-Sembel, Acria, Abashawl, Godaif and Maychehot have piped water system (Figure 1). The people of the ten villages mainly depend on farming and animal rearing for their daily livelihood, while most inhabitants of Sembel, Akria, Maychehot, Abashawl, and Godaif are government or private employees, and traders [19-22].
Study design and sampling
Descriptive cross-sectional study was conducted in fifteen locations in September 2019. Systematic random sampling was used in selecting the 50 households from each study area with the exception of Dembezawl, having only 40 households, resulting to a total of 740 households. Since this study was done instantaneously after the rainy season, all households were considered to have water holding containers and included in the sampling frame. During sample selection, all selected households were coded so as to avoid repetition. All households situated in all the study sites were eligible to be included in the study. Closed households or residences of non-consenting owners were not considered during household sampling.
Tools and materials
Dipper, 30 ml pipettes, vials, enamel tray, record forms, pen, pencil, eraser, note book, GPS for measurement of elevation, flash light, marker and adhesive tape for labelling were used in the field. In the laboratory, cages, tetramin, enamel tray, pipettes, 250 ml plastic cups with mesh, aspirator, freezer, silicate, dissecting microscope and zoo Taxa key for identification were used.
Ethical approval and data collection process
The paper received approval from Ministry of Health (MoH), Zoba Maekel, research ethical review committee. At the study sites, consent was obtained from the residents of selected households, then, a very careful investigation was done in every household. The data collection team tried to identify water holding containers which may harbour the immature stages of the mosquito indoor as well as outdoor. Using various materials and techniques, samples were collected from different containers and recorded in an entomological form (Figure 2). Data collection was finalized within ten days.
Standard dipping (300 ml) was done to collect the immature larvae and pupae from water containers having wide openings with >1 litters of water. Whereas pipetting (5 ml plastic pipette) was applied for smaller functional containers after permission has been granted from the owners. Collection from discarded objects like tins and small bottles was done by emptying to trays and collecting by pipettes.
All the larvae and pupae collected were put in loosely closed vials labelled with date, household number, location and container type. They were carefully transferred to the medical entomology laboratory at Asmara college of health sciences within the same day of collection. In the laboratory, they were classified according to their stages, location, container and date of collection. They were separated in to either Aedes or Culex genus. Tertramin was given to the larvae till they transformed to pupae, while the pupae were put in a netted cage. Morphological identification was done for all the emerged adults in a dissecting microscope using the zoo taxa key.
Data analysis
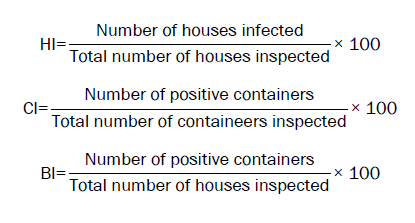
After data collection, data were entered into SPSS (version 20) and descriptive analysis was done in order to determine the breeding preference of the immature mosquito and productivity of different containers. The risk indices, House Index (HI), Container Index (CI) and Breteau Index (BI) for each site were calculated using Microsoft excel spreadsheet by the following formulas:
In the study, a total of 740 households in 10 villages of Zoba Maekel and 5 localities of Asmara, were assessed for the detection of Aedes mosquitoes breeds. In general, 1089 different kinds of water holding containers were identified in the study premises. From the assessed containers, 2759 immatures were collected, out of which, 88% were at their larval stage. From the total collected immatures, 664 were identified as Aedes mosquitoes either at a larval or pupal stage. At the end of the study, 276 Aedes and 816 culex mosquitoes emerged in to their adult forms out of the total collected. Which, 110 were confirmed as Ae. Aegypti and 166 were identified as other Aedes species. From this outcome, 87% of the inspected localities were found to be positive for the adult stage Aedes specie mosquitoes, out of which, 26% had Ae. Aegypti where as 80% were positive only for the other type of Aedes species or for both.
From their pupal stage, 1092 mosquitoes emerged in to their adult forms, accounting to 10% Ae. Aegypti, 15% other Aedes species and 75% culex mosquitoes. According to this, the primary vector mosquito Ae. Aegypti was discovered in four localities. Whereas, the mosquitoes classified as other Aedes specie was identified in 12 localities. In three areas, namely Adi-keshi, adi-guadad and Emveyto, both kinds of Aedes specie mosquitoes were identified. Out of the total studied localities, Embeyto (18%) and Ktmowlie (14%), had the highest number of positive houses for the vector mosquitoes (Table 1).
| Location | Total houses | Positive houses N (%) | Ae. Aegypti N (%) | Other Aedes species N (%) | Culex N (%) |
|---|---|---|---|---|---|
| Adi-Keih | 50 | 6 (11.76) | 40 (36.36) | 0 (0.00) | 8 (0.98) |
| Adi-Keshi | 50 | 4 (7.84) | 24 (21.82) | 36 (21.69) | 48 (5.88) |
| Adi-Guadad | 50 | 6 (11.76) | 15 (13.64) | 11 (6.63) | 41 (5.02) |
| Ktmowlie | 50 | 7 (13.73) | 0 (0.00) | 25 (15.06) | 110 (13.48) |
| Embeyto | 50 | 9 (17.65) | 31 (28.18) | 25 (15.06) | 55 (6.74) |
| Adi-Gebru | 50 | 2 (3.92) | 0.0 (0.00) | 7 (4.22) | 8 (0.98) |
| Tseazega | 50 | 1 (1.96) | 0.0 (0.00) | 1 (0.60) | 88 (10.78) |
| Geshnashim | 50 | 2 (3.92) | 0.0 (0.00) | 12 (7.23) | 96 (11.76) |
| Dembezawel | 40 | 0.0 (0.00) | 0.0 (0.00) | 0.0 (0.00) | 16 (1.76) |
| Gheremi | 50 | 1 (1.96) | 0.0 (0.00) | 2 (1.20) | 0.0 (0.00) |
| Godaif | 50 | 5 (9.80) | 0.0 (0.00) | 31 (18.67) | 179 (21.94) |
| Sembel | 50 | 0.0 (0.00) | 0.0 (0.00) | 0.0 (0.00) | 98 (12.01) |
| Abashawel | 50 | 2 (3.92) | 0.0 (0.00) | 3 (1.81) | 58 (7.11) |
| May-Chohot | 50 | 4 (7.84) | 0.0 (0.00) | 10 (6.02) | 5 (0.61) |
| Akria | 50 | 2 (3.92) | 0.0 (0.00) | 3 (1.81) | 6 (0.74) |
| Total | 740 | 51 (100) | 110 (100) | 166 (100) | 816 (100) |
Table 1. Adult Aedes mosquito identified and their species in the fifteen study sites.
From all the studied localities, a total of 1089 water holding containers, 20% indoor and 80% outdoor, were inspected as a potential breeding habitat for Aedes mosquitoes (Table 2). Among these, no container was found to be positive in an indoor setting, while 53 (6%) of the outdoor containers were found to contain the immature forms of the mosquito. Containers commonly preferred by the Aedes mosquitoes were plastic barrels (42%), tyres (21%), and metal barrels (15%) as containers made of clay presented no immature forms of the mosquito. Analysis of the most favourite breeding container using the Breeding Preference Ratio (BPR) evidenced that discarded tyres were the most preferable, followed by water tank, others, plastic barrels, metal barrels and jerricans.
| Container type | Indoor N (%) | Positive N (%) | Outdoor N (X%) | Positive N (%) | Breeding Preference Ratio (BPR) (Y/X) |
|---|---|---|---|---|---|
| Plastic barrel | 110 (51.16) | 0.0 (0.00) | 403 (46.11) | 22 (41.51) | 0.9 |
| Metal barrel | 41 (19.07) | 0.0 (0.00) | 169 (19.34) | 8 (15.09) | 0.78 |
| Jerrican | 11 (5.12) | 0.0 (0.00) | 67 (7.67) | 3 (5.66) | 0.74 |
| Discarded tyre | 27 (12.56) | 0.0 (0.00) | 86 (9.84) | 11 (20.75) | 2.11 |
| Clay | 2 (0.93) | 0.0 (0.00) | 21 (2.40) | 0.0 (0.00) | 0 |
| Water tank | 10 (4.65) | 0.0 (0.00) | 39 (4.46) | 4 (7.55) | 1.69 |
| Other* | 14 (6.51) | 0.0 (0.00) | 89 (10.18) | 5 (9.43) | 0.93 |
| Total | 215 (100) | 0.0 (0.00) | 874 (100) | 53 (100) |
*Bottles, jars, cans, flower vases, small plastic containers
Table 2. Combined larval and pupal positivity and breeding preferences by container type.
For the 120 Aedes pupae collected from all water holding containers, discarded tyres (40%) and plastic barrels (28%) were identified to be the most productive container types for the vector mosquito, followed by metal barrels, water tanks and others. Containers made of clay in this study had been found free for any stage of the vector mosquitoes, whilst jerricans were not productive even though they contained the larval form of the Aedes mosquitoes (Figure 3).
In analyzing the HI, CI and BI for Aedes larvae and pupae, a total of 740 houses were examined, of which, 51 of the households were found to be infested by Aedes immatures. The proportion of houses that were positive for this mosquito (HI) was highest in Embeyto (18%), followed by Kutmewlie (14%), Adi-keih (12%) and Adi-guadad (12%). From the 874 containers inspected, 53 were identified as Aedes mosquito habitats. Villages with highest CI were Embeyto (19%), Adi-keih (12%), Adi-Guadad (12%) and ketmowlie (11%), whilst the remaining villages gave relatively lower percentages. BI of the sites, which shows the number of positive containers for every 100 houses inspected was, similar to HI and CI, highest in Embeyto (20%); Ketmeulie and Adi-Guadad followed with 14% each. Over all, the villages with the lowest HI, CI and BI were Gheremi and Tseazega (Table 3).
| Location | Total houses | Positive houses | Total containers | Positive containers | HI | Cl | BI |
|---|---|---|---|---|---|---|---|
| Adi-Keih | 50 | 6 | 51 | 6 | 12 | 11.76 | 12 |
| Adi-Keshi | 50 | 4 | 50 | 4 | 8 | 8 | 8 |
| Adi-Guadad | 50 | 6 | 60 | 7 | 12 | 11.67 | 14 |
| Ktmowlie | 50 | 7 | 63 | 7 | 14 | 11.11 | 14 |
| Embeyto | 50 | 9 | 54 | 10 | 18 | 18.52 | 20 |
| Adi-Gebru | 50 | 2 | 53 | 2 | 4 | 3.77 | 4 |
| Tseazega | 50 | 1 | 52 | 1 | 2 | 1.92 | 2 |
| Geshnashim | 50 | 2 | 57 | 2 | 4 | 3.51 | 4 |
| Dembezawel | 40 | 0 | 44 | 0 | 0 | 0 | 0 |
| Gheremi | 50 | 1 | 57 | 1 | 2 | 1.75 | 2 |
| Godaif | 50 | 5 | 75 | 5 | 10 | 6.67 | 10 |
| Sembel | 50 | 0 | 62 | 0 | 0 | 0 | 0 |
| Abashawel | 50 | 2 | 63 | 2 | 4 | 3.17 | 4 |
| May-Chohot | 50 | 4 | 69 | 4 | 8 | 5.8 | 8 |
| Akria | 50 | 2 | 64 | 2 | 4 | 3.13 | 4 |
| Total | 740 | 51 | 874 | 53 | 6.89 | 6.06 | 7.16 |
HI: House Index; Cl: Container Index; BI: Breteau Index.
Table 3. Combined larval and pupil indices of Aedes species in the fifteen study sites.
In this study, the presence of dengue fever vectors was systematically investigated for the first time in this high altitude region of Zoba Maekel. Similar to the finding in mount Bizen, Eritrea back in 1945, the Aedes specie vectors were identified in 13 high altitude localities, out of which, four had the primary dengue fever vector Ae. Aegypti. Namely Adi-Guadad, Adi-Keih, Adi-Keshi, and Embeyto, elevated 2330 m, 2202 m, 2165 m, and 2109 m ASL, respectively. Generally, all positive localities elevation ranged from 2109–2349 m SL, which is similar to the findings in Mexico as of 2011. Even though emergence of dengue fever may not be only determined by climate; climatic changes are believed to contribute to its spread by creating conditions that can be favourable for the vector mosquito. In Asmara, in the last eight years, the average mean temperature has increased by the rate of 0.04°C per year. Over the period of 1880–2012, our planets temperature has increased by 0.85°C, besides, by the year 2100 average global temperature is expected to rise by 2.0°C. Considering this, dengue fever vectors have been projected to emerge in high altitude regions of Eastern Africa. As long as this climatic changes are believed to have a direct biophysical influence on viral replication, vector development and survival, it can be said there is a risk on proliferation of the vector in this highly elevated localities, given the climatic changes continues as projected. As so, further assessment on vectors viral transmission capabilities and studies considering local climatic conditions in relation to this vector born disease is needed.
In all the 13 areas, the vectors were found only in outdoor settings and the highest positivity was observed for plastic barrels followed by discarded tyres and metal barrels. This indicates the abundance of these containers in the studied localities and their capacity in harbouring the vector mosquitoes. Therefore, as long as presence of these water holding containers gives Aedes mosquitoes a chance to breed and as result increase their population, which increases risk of dengue fever transmission, proper control measures targeting these receptacles could have a significant result. Even though plastic barrels had the highest positivity, the most preferred breeding habitat, according to BPR, was identified as discarded tyres. Comparable study in India had similar findings, which the results, could be due to the way water is stored in discarded tyres, where its covered, dark, undisturbed and nutritious environment for the larvae in the presence of leaf litter and debris make it favourable for mosquito breeding. Other small containers and plastic barrels also had comparably higher BPR levels following discarded tyres. In these localities, small containers such as discarded cans, bottles, small plastic containers and others were found discarded randomly in the premises. This could allow water to be easily accumulated and create an open opportunity for mosquito breeding. Due to irregularity and shortage of water, residents in the different localities store piped or rain water in different water holding containers, mostly plastic barrels. Therefore, during summer, rain water is expected to be collected, so that it might supply the family for certain period of time. For that reason, containers are kept open under gargoyles, so as to reserve as much water as possible. Specially, at the end of the rainy season, the amount of rain gets scarcer and it takes longer for a barrel to get filled, leaving it open in outdoor for a longer period of time. This, possibly, creates a good opportunity for mosquito breeding and gives the off spring enough time to hatch and mature in to their adult forms without interruption. The lack of positivity in indoor containers in this study could have resulted because of the resident’s preference in placing containers holding water for drinking or food preparation inside their houses. Which is expected to be taken with good care and covered with a lid? These containers also being subject to frequent emptying and cleaning can also be key in interrupting mosquito development. This indicates that future prevention strategies focusing in increasing awareness of residents on the proper way of handling water reservoirs could have an effective outcome.
In this study outdoor discarded tyres and plastic barrels had the highest percentage of productivity which indicates that these materials harbour undisturbed stagnant water for a long period of time enough for the eggs to reach in to their pupal form. This is similar to the findings in Tanzania and Congo but somehow different to the studies in Kenya and Gash-Barka region of Eritrea. Where buckets, pots and metal barrels were the most productive containers. This can be due to variance in the commonly used water holding containers or their market availability in the different areas, even though other factors such as difference in climate, biotic and abiotic contents of the water or the material content of the containers should also be considered.
All indices used to assess the levels of Aedes specie infestations in this study showed, almost half of the localities had thresholds above the high risk arbovirus transmission levels indicated by the pan American health organization. Even though higher than these thresholds, the indices are lower when compared to results from the lowland region of Eritrea (elevation, 450-1800 m ASL). Which had an overall result for HI, CI, and BI as 67.3, 30.1 and 1,37.0 correspondingly. Similarly, these findings are lesser compared to Dire Dawa Metema and humera in Ethiopia, localities elevated 1191, 685 and 602 m ASL, in that order. Even though, the assessed indices of Aedes species are inferior to those discovered in lower altitude localities, the results indicate possibility of dengue virus transmission in these previously dengue fever free areas. Identification of this outcome in Godaif, and May-Chohot, localities found inside the capital city of Asmara, in particular makes the required intervening actions compulsory, taking in to consideration the likelihood of mosquito proliferation in an urban setting with time and its immediate health risk to the urbanites.
The dengue fever vector has been discovered in thirteen localities out of the fifteen studied, this finding delivers further evidence and data supporting the previous discovery of the potent dengue fever transmitting mosquito, Ae. Aegypti, in high altitude areas of Zoba Maekel, namely Shmangus-Tahtay, and Dembe-Aditsegede, as of 2018; and consistent suspicion of dengue fever from the respective health care facilities. This offers base line material for further in depth studies and creates new perspective on the risk of dengue fever transmission in this area. Discovery of domestic outdoor water receptacles as a primary habitat for the development of the potentially capable dengue virus transmitting mosquito demonstrates possibility of easy human to human transmission once the disease presents itself in this area. Therefore, future control strategies could focus in improving awareness of residents in handling outdoor water storage containers and elimination of the most preferred and productive habitats such as discarded tyres.
The paper received approval from Ministry of Health (MoH), Zoba Maekel, research ethical review committee.
The authors declare that they have no competing interests regarding this publication.
The research team would like to thank the Orotta collage of medicine and health science, school of public health, administrators of all localities, community health workers, and consenting household owners for their contribution.
Mr. Meles Gebreyesus and Rusom aile from Zoba Maekel’s malaria control program likewise deserve our earnest appreciations for their full cooperation.
We would also like to express our deepest gratitude to Mr. Bereket Kidane and Kudus Zekarias from zonal administration of Zoba Maekel, GIS Unit; Mr Bereket Berhane and Isaak Fseha, Eritrean |Metrology; Mr. Asrat Haile, Eritrean ministry of agriculture; and also Mr Dawit G. Weldemariam for their support.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]