e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
KM Shah Dental College and Hospital, Piparia, Waghodia, Vadodara-391760, Gujarat, India
Received: 07/03/2013 Revised: 03/04/2013 Accepted: 09/04/2013
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
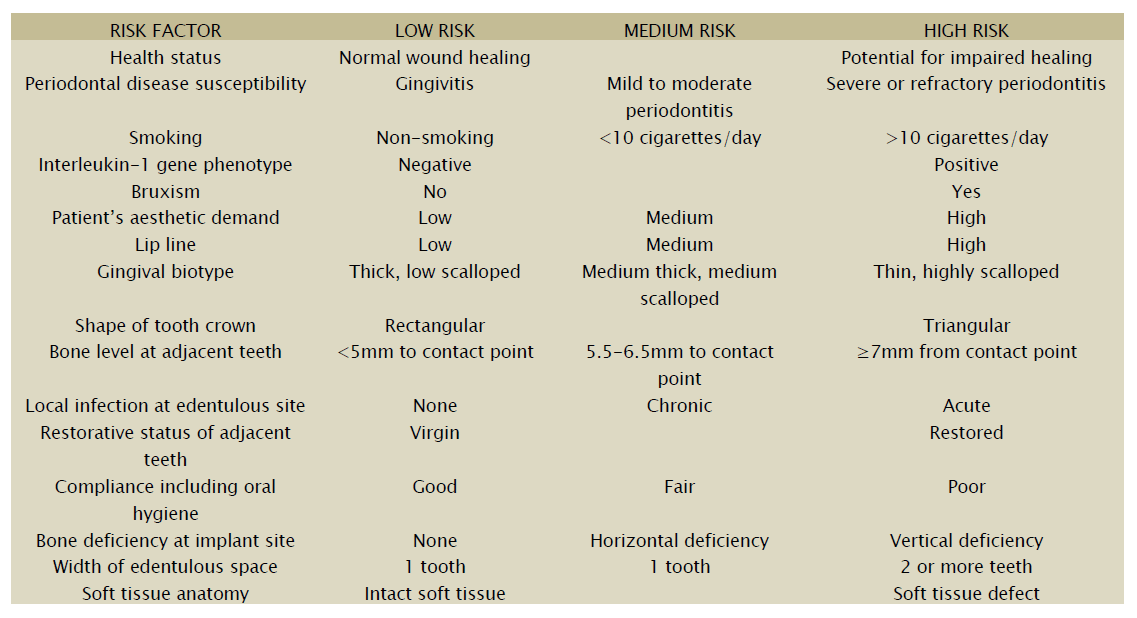
In today’s world, with the gaining popularity of dental implants among patients, there is an increasing need for understanding the case selection criteria so that dental implants can be placed with high success. Indiscriminate implant placement can lead to major complications during the post-operative or prosthetic phase of treatment, leading to achieving compromised results. There are many complicating and risk factors involved that can dramatically change the treatment modality for teeth replacement. This review paper tries to throw light on some of the issues that should be addressed during the decision making phase of implant therapy.
dental implants, case selection, treatment planning
Modern comprehensive dental care has to include the consideration of dental implants. Currently, substantial scientific and clinical evidence has become available to help the understanding of factors enhancing or compromising treatment success with regard to functional and aesthetic success. In relation to implant surgery, careful risk assessment should also be made. In the edentulous jaw, implants supporting fixed or removable prostheses will more frequently be inserted in anterior regions where there are more favourable alveolar bone dimensions and quality. In partially edentulous patients, implants are more likely indicated in posterior regions with less favourable anatomic conditions. The volume of alveolar process may also be substantially reduced due to periodontal disease. Hence following issues should be considered prior to implant placement.
An understanding for patient’s needs, socioeconomic background, general medical condition etc., is a prerequisite for successful therapy.1 There should be a complete assessment of the patient’s chief complaint and expectations, dental history, motivation and compliance, habits (e.g., smoking, tobacco chewing) [1]. Optimal individual treatment results may only be achieved if the patient’s demands are in balance with the objective evaluation of the condition and the projected treatment outcomes.
Assessment of mouth opening should be done, as instrumentation involved with implant therapy need sufficiently wide mouth opening. Aesthetic characteristics like smile line, lip line, and facial midline should be evaluated in patients needing tooth replacement in aesthetic zone [2].
Residual infections in the alveolar bone (e.g. failed endodontic treatment), non-vital teeth especially those adjacent to edentulous space, caries, overhanging restoration margins etc., should be treated before considering implant therapy as a treatment option. Analysis of static and dynamic aspects of patient’s occlusion should be analysed [3]. These include adequacy of vertical dimension of occlusion, maxilla-mandibular relationship, overjet, overbite, stability in habitual occlusion, centric relation, canine guidance etc [3].
Sites without aesthetic implications
Clinical width and height of alveolar process should be evaluated. Bone sounding can be done for bone mapping to evaluate the bucco-lingual width of alveolar process.
3-D space assessment can be used for evaluation of the condition of the adjacent teeth and their surrounding hard and soft tissues [1].
Accurate space assessment is difficult intraorally, hence articulated mounted casts should be used. When multiple adjacent teeth are to be replaced, diagnostic wax–up can be very useful. Diagnostic wax-up also help in alignment and parallelism of implants to be placed [1].
From restorative point of view, edentulous spaces to be restored with implants should ideally have mesio-distal width of natural teeth that would normally be there. In periodontally compromised patients, width of edentulous spaces is usually reduced due to pathologic migrations. As a general guideline, a minimum vertical distance of 4mm, from crestal mucosa to implant site, is required for a straightforward implant placement [1]. When tooth is lost due to periodontitis, this distance is usually more. This may result in overlong implant restoration.
Sites with aesthetic implications
Most visible sequel of periodontal disease is its direct impact on aesthetic appearance. This leads to overlong clinical crowns and flattening of originally scalloped course of gingival line, including loss of papillary tissue, leading to ‘black triangles’. This problem is pronounced in patients with ‘thin biotype’. In case of localised periodontal disease, abrupt changes occur in vertical tissue height between neighbouring teeth. All these issues create major aesthetics problem during prosthetic phase of implant therapy.
Elements of local, implant specific examination in aesthetic zone include smile line (high, medium, low), periodontal examination, inter-proximal bone height, bone anatomy of existing/anticipated edentulous ridge, course of gingival line with respect to cementoenamel junction of adjacent teeth and osseous ridge, gingival phenotype (‘flat thick’ v/s ‘scalloped thin’),[4] shape of anatomic crowns (‘square’ v/s ‘triangular’), [4] length to width ratio of clinical crowns [4], occlusal parafunction, and width of edentulous space (identification of edentulous ridges that do not correspond to volume of respective missing teeth).
Maxilla[5]
In areas edentulous since many years, the maxillary sinus tends to expand into the remaining alveolar ridge, due to lack of functional stimuli from teeth and due to negative pressure during inspiration. Overtime, pneumatisation may cause residual alveolar bone to resorb as a result of continuous expansion of maxillary sinus along with horizontal and vertical forces. In anterior maxilla, the incisive foramen travels anterior with resorption of maxilla.
Mandible[5]
In highly resorbed anterior alveolar ridge, the genial tubercles may be found superior to residual crest and mental foramen may also travel close to the crest. In some patients, the mental nerve before exiting through mental foramen, may present with an anterior loop that runs infero-medial-lateral or inferior to mental foramen. This loop may extend 1-7 mm anteriorly, depending on size of mandible. The inferior alveolar nerve is present approximately 3mm apical to 1st molar.
It is mandatory to do radiographic examination as it serves to
Ascertain that implant treatment is an appropriate treatment given the condition of remaining teeth.
Make certain that bone height and width are sufficient for implant placement.
Provide measurements so that implants can be inserted without damaging neighbouring structures.
Make implant procedure a safe procedure.
The different radiographic methods used are:-
Intraoral Radiography
It is part of primary investigation as diagnostically important structures are clearly visible in an intraoral periapical radiograph.5 Paralleling technique should be used for intraoral radiography. Some overlapping between adjacent fields should be there so that the entire edentulous area is covered [5].
Panoramic Radiography
It is also a part primary investigation as it gives a quick estimate of bone height.5 However, this technique involves high chances of distortion, which may be visible in dentulous areas, but is not apparent in edentulous regions.5 This may lead to misjudgement of distances within jaws.
Tomography
It is used to obtain cross-sectional images i.e. perpendicular to curvature of jaw bone at the intended implant sites. It is the best way to assess width and height of bone available for implant placement. Three types of tomography are present.
Conventional Tomography
It is done after the area of interest is identified from a panoramic radiograph. It permits image layers of 2-4mm width.
Computed Tomography
This type of radiography is associated with high radiation doses and is not ideal for examination of dentate patients. Its use is justified only when several edentulous regions within the same jaw need to be examined [6].
Digital Volume Tomography
This technique is associated with low doses of radiation compared to computed tomography. Radiation doses can be kept to minimum by exposing smallest possible volume. Images obtained can be reconstructed so that layer images of exposed volume appear on screen, giving a three dimensional image [6].
Though a very high success rate of implant therapy has been reported in literature, it is still imperative to do follow a proper case selection protocol for implant therapy so that the outcome of a dental implant can be successfully predicted. A meticulous comprehensive examination of implant candidates is crucial and should include a patient centred and indication specific risk assessment to achieve favourable short and long term treatment outcomes with regard to function and aesthetics.