e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
Department Of Oral & Maxillofacial Surgery, Indira Gandhi Govt. Dental College, Jammy.
Received: 11/08/2014 Revised: 22/08/2014 Accepted: 28/08/2014
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
The present study was done to evaluate the effectiveness of distraction osteogenesis as a treatment modality in case of craniofacial deformity associated with cleft lip and palate patients and to suggest a protocol for distraction osteogenesis for midface and dentoalveolar segments in cleft lip and palate patients. Seven patients with cleft lip and palate having midfacial deficiency and falling in ASA grade 1 and ASA grade 2 categories were selected and taken up for the necessary treatment with the use of a Le Fort 1 osteotomy and application of Rigid external distractor (RED). The distraction was carried out over a period of 6-13 days at a rate of 4.0 mm per day for four patients, 1.5 mm per day for one patient (split over twice daily) and 2.0 mm per day for two patients. Advancement of the segment achieved at the end of one month fell in the range of 14 mm – 18 mm and 4 mm - 16 mm at the end of six months. Distraction osteogenesis proved to be an effective treatment modality in case of craniofacial deformity associated with cleft lip and palate patients. We have also suggested a protocol for distraction osteogenesis for midface and dentoalveolar segments in such patients.
Rigid external distractor (RED); Le Fort 1 osteotomy; Cleft lip-palate patients
Patients with repaired cleft lip and palate present with large osseous defects of the alveolus and midface hypoplasias [1]. In these patients, normal growth of maxilla may be hindered because of early repair and the consequent scarring. However mandibular growth is normal or not much hindered. Midface deficiency in these patients is normally seen in all three planes. In addition there is absence of maxillary and alveolar bone, scarring, residual fistulas, and dental anomalies [2].
Traditional orthognathic surgery and craniofacial reconstruction have gained generalized acceptance but severe limitations have been seen. One of the major limitations is the inability of the soft tissue to stretch leading to relapse. Others include pharyngeal constriction, speech problems, compromised function, damage to the tooth buds, need for excessive hardware, selective age group and infection [3]. Traditional orthognathic surgery and craniofacial reconstruction, although sometimes successful in obtaining stable occlusal relationships, often fall short of expectations with respect to facial balance and esthetics [4].
Distraction osteogenesis –seems to solve most of these problems. As it is a well-known fact that bone is a regenerative organ and has an inherent capacity to restore its form and function, distraction osteogenesis utilizes this capacity of bone as its basic principle along with the soft tissue improvement.
Distraction Osteogenesis is the process of generating new bone in a gap between two bone segments in response to the application of graduated tensile stress across bone gap [5].
Using easily controlled mechanical conditions; it is possible to generate a new bone and its spatial orientation to form a structural part of bone [6]. The aim of this study is to evaluate the effectiveness of distraction osteogenesis as a treatment modality in case of craniofacial deformity associated with cleft lip and palate patients and to suggest a protocol for distraction osteogenesis for midface and dentoalveolar segments in cleft lip and palate patients.
Amongst the cleft lip and palate patients who reported to the Department of Oral and Maxillofacial surgery, 7 cases having midfacial deficiency and falling in ASA grade 1 and ASA grade 2 categories were selected and taken up for the necessary treatment with the use of a Le Fort 1 osteotomy and application of Rigid external distractor (RED). Complete case history was taken along with general physical examination and presence of syndromes was looked for.
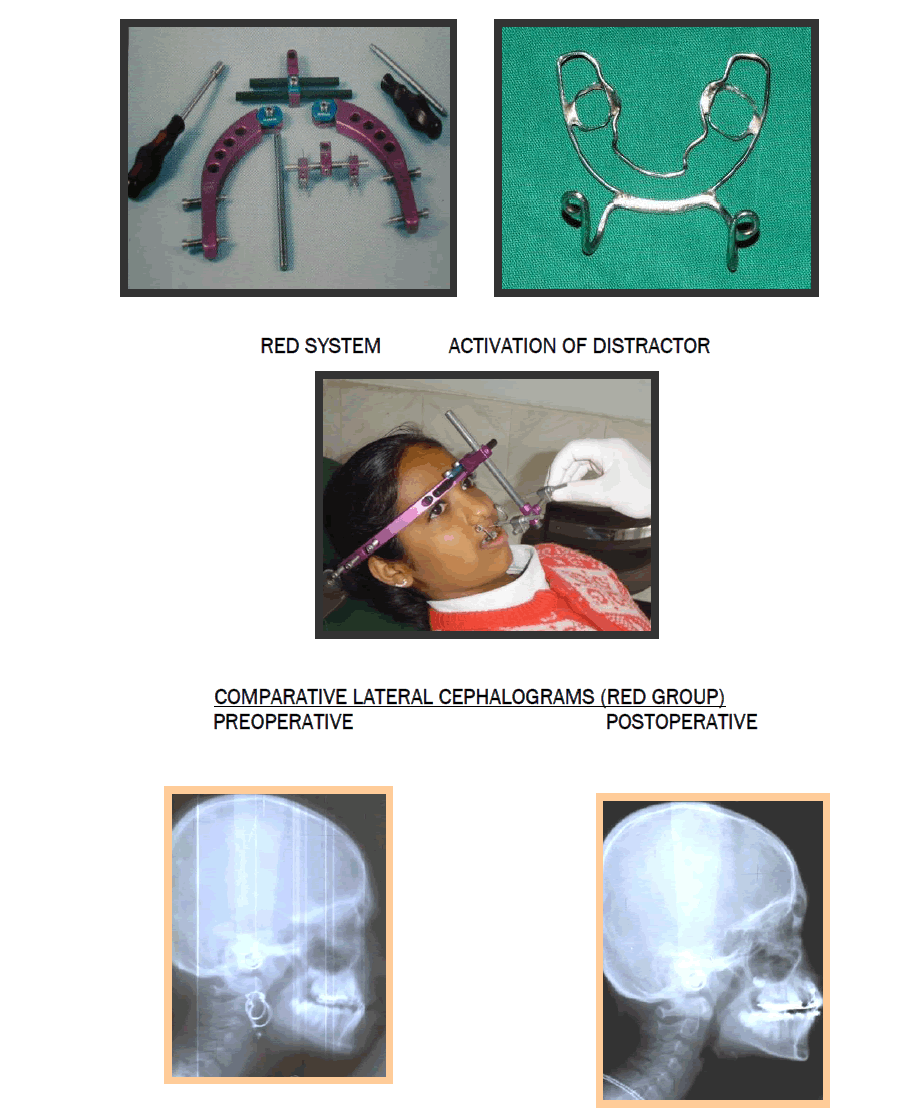
Photographic records were maintained preoperatively, intraoperatively, during retention period and postoperatively in all the cases. Preoperative lateral cephalograms and orthopantomograms were taken to evaluate the midface deficiency and occlusal radiographs and intraoral periapical radiographs were taken to determine the position of the roots of the teeth. Immediate Postoperative lateral cephalograms, lateral cephalograms at the end of 1 month and lateral cephalograms at the end of 6 months were taken for the evaluation of advancement.
Surgical Techniques
In Operation theatre, after Intubation throat pack was placed in all patients.
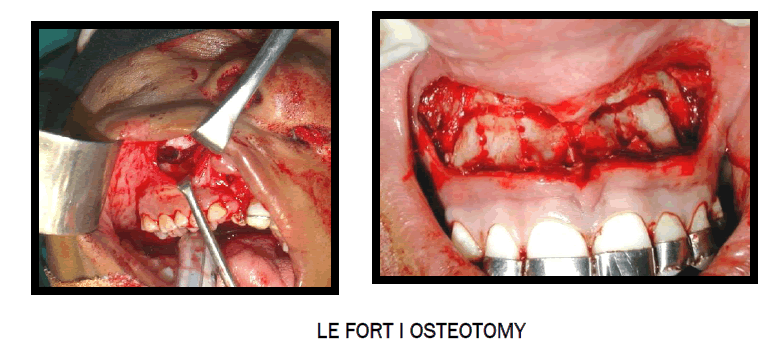
Le Fort 1 Osteotomy:
The oral incision was placed high in the mucobuccal fold of the upper lip, and it extended from the zygomaticomaxillary buttress region across the midline. The incision traversed the mucosa, the muscles attached to the lateral wall of the maxilla, and the periosteum. By subperiosteal dissection to the orbital rim, the infraorbital nerve was exposed and protected. The direction of the posterior dissection was posterior and inferior to the zygomaticomaxillary buttress to the pterygoid plate (This technique was followed in six patients who underwent Le Fort 1 osteotomy and distraction. In one patient the two vertical incisions were placed in the region of first molar and through the tunneling approach, dissection was carried out).
The osteotomy was initiated at the zygomaticomaxillary buttress region about 5 mm superior to the second molar to minimize the risk of devitalisation of teeth. The posterior osteotomy was directed inferiorly as it proceeded posteriorly from the zygomaticomaxillary buttress to the junction of the maxilla and the pterygoid plate in order to minimize the risk of damaging the maxillary artery. Then the osteotomy of the maxillary sinus was completed from inside to outside. Similar procedure was carried out on the contralateral side.
Now the bone of the nasal septum and vomer from the maxilla was freed of the cartilage with the help of a septal osteotome. The osteotome was placed at the piriform rim and directed posteriorly and inferiorly along the lateral nasal wall towards the perpendicular plate of the palatine bone and the palatine bone was sectioned off.
Now the maxilla was separated from the pterygoid plates. A curved osteotome was directed medially and anteriorly at the lowest part of the junction of the maxilla and the pterygoid plate. The osteotome was malleted to achieve bony separation and the tip was palpated after doing this. In the end, the head frame was centralized and attached to the cranium. Then the patient was extubated and shifted to recovery.
Distraction protocol included Latency period of 2 days and consolidation period of 3-6 months. Regular follow up was done with splints and distracters.
Out of seven patients treated, four (57.1%) were males and three (42.9%) were females. The average age for males was 16 years & the average age for females was 14 years.
Distraction was carried out at a rate of 4.0 mm per day for four patients and at a rate of 1.5 mm per day for one patient (split over twice daily). Two patients were distracted at the rate of 2.0mm per day. The distraction was carried out over a period of 6-13 days (avg 7.6 days). The total activation done varied from 20-28 mm (avg 23.2 mm). All the patients were followed up for a period of minimum six months. (Table 1)
Advancement of the segment achieved at the end of one month fell in the range of 14mm - 18mm (avg 15.6 mm). Advancement at the end of six months was 4mm - 16 mm (avg 11.6 mm).
All the patients showed some amount of relapse that ranged from 2mm – 11 mm (avg 4.6 mm) after which the segments were stable. (Table 2)
One (14%) patient showed poor compliance. Five (71%) patients were satisfied with the results and one (14%) was partially happy. Relapse within normal limits (<5mm) was seen in four (57.1%) patients. One (14%) patient showed a relapse of 11 mm. One patient had pin tract infection. Early consolidation was seen in two (28%) patients. Loosening of splint was seen in one (14%) patient. Tissue trauma (irritation of the tissue with the splint) was seen in one patient.
However six (85%) patients showed definite improvement in their profile and had better esthetics compared to the preoperative picture.
Cleft lip and palate is a condition that is fairly common in India. It is one of the most common congenital defects found all over the world. It has been estimated that 25% - 50% of all patients born with unilateral cleft lip and palate will be candidates for maxillary advancement to correct functional deformities and improve aesthetic facial proportion.7 Other studies put this incidence to 25%-60% [8,9].
Patients with severe cleft maxillary deficiency are difficult to treat with traditional surgical/orthodontic approach. These patients present with maxillary hypoplasia in all the three dimensions along with thin and structurally weak bones. These include severe malocclusion, which results in compromised mastication, speech abnormalities and pharyngeal airway constriction [10].
Current protocols in treatment of maxillary hypoplasia rely upon a surgical/orthodontic approach, including a Le Fort I maxillary advancement with concomitant fistula closure and maxillary and alveolar bone grafting [11]. Various authors have reported the long-term results of cleft patients with maxillary deficiency treated by such methods. Mean advancement in these patients has averaged between 5mm to 7mm and mean long-term horizontal relapse ranges from 20% to 25% [12].
In addition, the age group in which these procedures can be carried out is limited. Also in the patients treated with cleft orthognathic surgery with a Le Fort I osteotomy mostly have tendency for medial, superior, and posterior drift of lesser segment in some patients. To combat this relapse pattern, planned surgical overcorrection, and long-term orthodontic retention techniques are required.
Distraction seems to overcome most of these problems. One of the greatest advantages of distraction osteogenesis is that it can be done at any age (as early as 5 years) [13].
In this study, 7 consecutive patients underwent maxillary advancement at Le Fort I level using rigid external distractor (RED). In 1 patient, an acrylic and wire splint covering the occlusal surface was prepared. But various problems were encountered in such a splint including hygiene and comfort and patient complained of difficulty in eating.
In 6 patients, prefabricated 1.0 mm stainless steel wire splint was used for retention intraorally. The advantages of such a splint were as it was custom designed, which is imperative, especially in patients with clefts that present with severe dental malpositions and collapsed cleft arch segments. It was also hygienic, comfortable and nontraumatic.
One patient in the RED group showed a severe relapse of 11 mm. This was attributed to the non-compliance during therapy and retention period involving facemask traction. RED uses a skeletally fixed device that allows rigid predictable control over the distraction process.
The premaxillary and interdental distraction patients showed no relapse and the distracted segment was stable at the end of 6 months.
Distraction was carried out at a rate of 0.75mm in the morning and 0.75 mm in the evening after a latency period of 4 days in one patient. A retention period of 4 weeks was given. The time of post distraction cephalometric analysis was 6 months. This is a protocol that is followed in most centers [14].
However, we did not achieve sufficient advancement. This was attributed to a longer latency period and early consolidation of callus. To overcome this problem, we modified our protocol. In 2 patients, distraction was carried out at a rate of 1 mm in the morning and 1 mm in the evening after a latency period of 4 days. Still the problem persisted. In 4 patients of the RED group, distraction was done at a rate of 2mm in the morning and 2mm in the evening after a latency period of 2 days. The device was kept in retention for 4 weeks. Mean advancement achieved at the end of 6 months in these patients was 12 mm. This was within the presurgical assessment limits.
With the use of RED, we can now gradually and in a very stable fashion reposition a hypoplastic maxilla to the exact horizontal and vertical position desired. The patients create their own autogenous bone during this process eliminating the need for both the donor site and the need for rigid internal fixation hardware.15 The use of RED has allowed rigid control over the distraction process and has allowed us to follow our surgical and esthetic guidelines for the reconstruction of these patients by correcting the maxillary and soft tissue discrepancy in the region of hypoplasia only. The expansion of the soft tissue facial mask yields the most pleasing long-term aesthetic facial balance and harmony, particularly in cleft patients [12].
The only limitations we encountered with RED include presence of adequate dentition, either primary or secondary, for fixation of intraoral splint as well as ability of the patient to wear the device which is in accordance with those in a study conducted by Meazzini et al [16].
In this study, we tried to evaluate the effectiveness of distraction osteogenesis as a treatment modality in case of craniofacial deformity associated with cleft lip and palate patients and we got encouraging results. The study has also tried to suggest a protocol for distraction osteogenesis for midface and dentoalveolar segments in cleft lip and palate patients.