e-ISSN: 2322-0139 p-ISSN: 2322-0120
e-ISSN: 2322-0139 p-ISSN: 2322-0120
1Departments of Biochemistry, Faculty of Basic Medical Sciences, Ladoke Akintola University of Technology, Ogbomoso, Nigeria.
2Departments of Physiology, Faculty of Basic Medical Sciences, Ladoke Akintola University of Technology, Ogbomoso, Nigeria.
Received date: February 15, 2018; Accepted date: February 21, 2018; Published date: March 10, 2018
Visit for more related articles at Research & Reviews: Journal of Pharmacology and Toxicological Studies
Antineoplastic drugs are well known for their abilities to induce varying degrees of toxicities and predispose to cardiovascular related disease states.
This study, therefore evaluates the effects of Doxorubicin (Dox) (3 mg/kg body weight) and Etoposide (Etop) (3 mg/kg body weight) alone and in combinations at 12 and 24 h intervals on plasma lipid profiles and paraoxonase-1. Lipid peroxidation, superoxide dismutase (SOD), glutathione peroxidase (Gpx) and reduced glutathione (GSH) in selected male rat organs were also evaluated. The results were analyzed using One-way ANOVA followed by post hoc tests.
Hypocholesterolemia characterized the effects of Etop alone and in combination with Dox at 12 h, while at 24 h interval hypercholesterolemia was observed in the combined group. Both drugs induced significant hypertriglyceridemia except at 12 h combination with significant hypotriglyceridemia. Individually, the drugs significantly reduced HDL-cholesterol (HDL-C) contrarily to up-regulation when combined. HDL-triacylglycerol, phospholipids and paraoxonase- 1 activities were significantly reduced in all the treated groups, compared with the control. Dox markedly elevated lipid peroxidation in liver and heart, but repressed by Etoposide in the heart and erythrocyte. In combination, Etop at both time intervals ameliorated Dox-induced lipid peroxidation. All treatments elicited significant reduction in liver and erythrocyte GSH levels except heart with significant increase. The treatments significantly depressed hepatic SOD activities while moderating GPx activities in all the organs studied.
This study shows that the derangements in the lipid profile are a common factor for the potential of the both drugs to predispose to cardiovascular diseases than the observed antioxidant status.
Antineoplastic, Cardiovascular disease, Lipid profile, Antioxidant Enzymes, Lipid peroxidation.
Cancer is a disease at a cellular level involving heritable disorders in cellular control mechanism. It is a manifestation of etiologic and pathogenic disturbances in the mechanisms that defies normal control of cell division, differentiation and homeostasis [1]. In the past years, biomedical research has put in significant efforts in finding out its cure, in spite of this cancer have been claiming lives.
Chemotherapy has made dramatic progress in recent years in reducing the morbidity and mortality from all forms of cancer [2]. It is a common and potent method for the treatment of different types and stages of cancer and is used to prevent its recurrence after surgery [3]. The chemotherapeutic options for patients now include increasingly complex combinations of medications, and they are very effective against cancerous cells because of the ability to interfere with rapidly dividing cells. These medications are likely to have significant toxic effects on the patients. Meanwhile [2], reported that cancer patients undergoing chemotherapy are most often severely ill. If these effects are, however understood, it will lead to a more effective management of cancer patients.
Etoposide and Doxorubicin are examples of such drugs that are employed as chemotherapeutic agents. Etoposide (C29H32O13) is a semisynthetic drug that is derived from podophyllotoxin employed in the treatment of certain neoplastic diseases. It is an inhibitor of DNA topoisomerase II, whose effect seems to appear mainly in the G2 phase of the cell cycle in human cells. As a chemotherapeutic agent, there is a need for its repetitive high doses as a result of its poor solubility and a very short half-life [4,5]. Doxorubicin, on the other hand, is an anthracycline with a broad spectrum of antibiotic that possesses antitumor activities against a wide range of human cancer with a speculative cardiotoxic potential [6]. It had been used to treat several hematologic and solid malignancies [2]. Its cardiotoxicity have been linked to the formation of free radicals and subsequent oxidative stress [7].
The effects of these chemotherapeutic agents on lipid metabolism and organ antioxidant enzymes still remain largely enigmatic. The present study therefore is aimed at studying the effects of single or combined treatments of Etoposide and doxorubicin on lipid metabolism and antioxidant enzymes of selected organs.
Test materials
Doxorubicin and Etoposide used for this study was purchased from an authorized Pharmaceutical Shop in Ogbomoso, Oyo State, Nigeria. The two drugs were then reconstituted with normal saline to obtain a stock concentration of 10 mg/ml.
Chemicals
Cholesterol and triacylglycerol kits were produced by Fortress Diagnostics Limited, Northern Ireland, United Kingdom. All other reagents and chemicals are of analytical grade and were obtained from Sigma Chemical Co. St Louis, MO., USA.
Experimental animals: In an in vivo experimental study to examine the toxic effect of doxorubicin and Etoposide, twenty (20) male albino rats of the Wistar strain weighing between 130–150 g were purchased from the Animal House, Department of Biochemistry, Ladoke Akintola University of Technology, Ogbomoso, Oyo State, Nigeria. The rats showed no visible signs of diseases or injuries. The rats were acclimatized for two weeks in the experimental Animal House of the Department of Biochemistry, Ladoke Akintola University of Technology, Ogbomoso and were fed with commercial rat pellets from Vita Feeds (Ibadan, Oyo State, Nigeria) and given water ad libitum. Animals were humanly cared for according to the guidance for care and used of experimental animals approved by Faculty of Basic Sciences Animals Ethic Committee, Ladoke Akintola University of Technology. Animals were randomized into five experimental treatment groups of five rats each.
Animal grouping and treatment
Group A serve as control and received normal saline every other two days for 15 days intraperitoneally (ip). Groups B received 3 mg/kg doxorubicin and Etoposide respectively through ip route, while groups D and E was exposed to 3 mg/kg of both drugs at 12 hours and 24 hours interval respectively via ip every other two days for 15 days as shown below.
Group I: normal saline
Group II: 3 mg/kg doxorubicin
Group III: 3 mg/kg Etoposide
Group IV: 3 mg/kg doxorubicin + Etoposide (12 hours interval)
Group V: 3 mg/kg doxorubicin + Etoposide (24 hours interval)
At the end of 15 days of the exposure period, blood was collected from the animals into heparinised tubes by cardiac puncture under light ether anesthesia after an overnight fast. The blood samples were centrifuged at 5000 rpm for 10 min to separate plasma and red blood cells.
Tissue sampling
Heart, Liver and Kidney were carefully dissected and washed in ice-cold 1.15% KCl solution. The tissues were homogenized in homogenizing buffer (50 mM Tris-HCl with 1.15% KCl of pH 7.4) using Teflon head Potter-Elvejhem homogenizer. The homogenate was centrifuged at 10,000 g for 10 min in a refrigerated centrifuge to obtain the post mitochondrial supernatant fraction. The supernatant was used for the evaluation of enzyme activities.
Plasma and lipoprotein lipid profiles
Plasma cholesterol and triacylglycerol concentrations were determined with commercial diagnostic kits obtained from Fortress Diagnostic, UK. High density lipoprotein (HDL) and low density lipoprotein + very low density lipoprotein (LDL + VLDL) cholesterol and triacylglycerol were also determined using the same commercial kits after LDL and VLDL were precipitated with heparin-MnCl2 solution. Determination of Phospholipids in plasma and lipoproteins followed the established procedure described by Stewart [8], after the phospholipids have been extracted according to the method of Rose and Oklander [9].
Assay of paraoxonase activity in the plasma
The paraoxonase activity of PON1 was determined using paraoxon (O, O-diethyl-o-p-nitrophenylphosphate) as the substrate. The increase in absorbance at 405 nm due to the formation of 4-nitrophenol following the hydrolysis of paraoxon was measured as described by Furlong [10]. The molar extinction co-efficient of 18050 M-1cm-1 was used to calculate enzyme activity.
Tissue lipid peroxidation and antioxidant enzymes
Lipid peroxidation was evaluated by measuring thiobarbituric reactive oxygen species (TBARS) in form of MDA using the method described by Varshney and Kale [11]. The method of Beutler [12] was employed in estimating the level of reduced glutathione in tissue homogenates. Glutathione peroxidase activity was evaluated using the method of Rotruck [13]. Superoxide dismutase (SOD) activity was evaluated using Fortress diagnostic kit which employed Arthur and Boyne (1985) [14], method. This method employs xanthine and xanthine oxidase to generate superoxide radicals which react with 2-(4-iodophenyl)-3-(4-nitrophenol)-5- phenyl tretrazolium chloride (I.N.T) to from a red formazan dye. One unit of SOD is that which causes a 50% inhibition of the rate of reduction of INT under the conditions of the assay.
Statistical protocol
Results were expressed as mean ± SD. The levels of homogeneity among the groups were assessed using Analysis of Variance (ANOVA). Where heterogeneity occurred, the groups were separated using Tukey Test. All analyses were done using Graph- Pad Prism® version 6.
Table 1 shows the effects of doxorubicin and Etoposide on plasma cholesterol and triacylglycerol concentration. Etoposide administered alone (3 mg) and in combination at 12 h time interval, led to a significant decline in the plasma cholesterol level. On the other hand, at 24 h time interval, a significant hypercholesterolemia was induced. This is similar to what was observed in plasma triacylglycerol concentration following 3 mg doxorubicin treatment alone, which led to a significant induction of hypertriglyceridemia.
| Groups | Cholesterol (mg/dl) | Triacylglycerol (mg/dl) | Paraoxonase activity (U/ml) |
|---|---|---|---|
| I | 92.86 ± 5.39 | 42.91 ± 2.70 | 153.9 ± 0.55 |
| II | 94.51 ± 2.72 | 91.96 ± 2.63 | 134.6 ± 0.10 |
| III | 71.65 ± 3.11 | 49.81 ± 2.32 | 135.1 ± 0.63 |
| IV | 38.14 ± 6.58 | 35.67 ± 2.63 | 147.7 ± 1.23 |
| V | 165.22 ± 25.03 | 53.55 ± 6.76 | 125.4 ± 0.48 |
Table 1: Effects of Doxorubicin and Etoposide on Rat plasma lipid profiles and Paraoxonas-1 in Rats.
The effects of both drugs on lipoprotein lipid profiles were depicted in Table 2. HDL cholesterol concentration was down-regulated by both doxorubicin and Etoposide when administered separately, contrarily to up-regulation when administered together at both 12 and 24 h intervals. Significant reductions in HDL triacylglycerol concentration were observed in all treated groups when compared with the control group. Similar reductions were obtained in the HDL phospholipid concentration following administration of doxorubicin and Etoposide either singly or in combinations.
| Groups | HDL-C (mg/dl) | HDL-T (mg/dl) | HDL-P (mg/dl) | LDL+VLDL-T (mg/dl) |
|---|---|---|---|---|
| I | 58.23 ± 6.26 | 123.34 ± 7.96 | 5.71 ± 0.59 | 22.83 ± 1.83 |
| II | 42.83 ± 2.80 | 61.27 ± 8.43 | 4.43 ± 0.34 | 36.59 ± 3.85 |
| III | 45.44 ± 3.61 | 98.40 ± 8.04 | 4.80 ± 0.25 | 31.16 ± 2.47 |
| IV | 63.37 ± 3.56 | 65.13 ± 4.89 | 3.81 ± 1.15 | 88.17 ± 4.56 |
| V | 70.17 ± 5.80 | 57.95 ± 1.93 | 3.51 ± 1.24 | 67.73 ± 2.30 |
Table 2: Effects of Doxorubicin and Etoposide on Rat Lipoprotein lipid profiles.
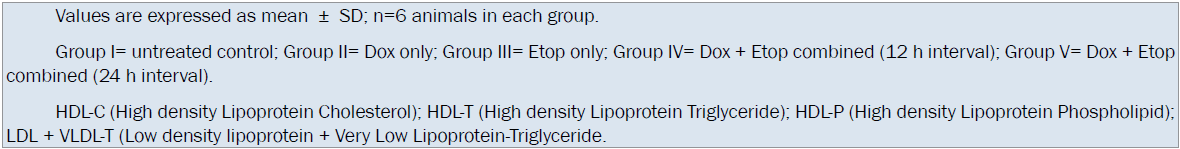
LDL+VLDL lipoprotein fraction presents an up-regulation of LDL+VLDL triacylglycerol concentration in all the treated groups as shown in the Table 2. This up-regulation became significant when both drugs were administered together at both 12 and 24 h intervals of administration when compared with the control group.
Both drugs either administered separately or combined at both 12 and 24 h intervals as depicted in Table 1 significantly reduced the activities of plasma PON-1 enzyme when compared with the control.
Dox exposure to rat was found to significantly induced increase in MDA levels in the heart (P<0.01) and liver (P<0.0001). The kidney MDA levels showed significant reduction (P<0.0001) while no significant difference were observed in Erythrocyte MDA levels. Etoposide alone reduced significantly Heart and Kidney MDA levels while no significant differences were observed in Erythrocyte and Liver when compared with the control group. Co-administration of Dox and Etop at both intervals did not induce significant changes (P>0.05) in the Heart and Liver MDA levels when compared with the control group. Kidney MDA levels at both intervals of co-administration showed significant decrease while significant reduction of Erythrocyte MDA levels was observed in 12-h intervals when compared with the control group (Figure 1).
Exposure to both drugs singly or in combination significantly reduced the activity of Liver SOD while no significant Heart, Erythrocyte and Kidney SOD activities were observed excerpt significant increase when the drugs were combined at 12-h interval (Figure 2).
Figure 3 shows that Dox alone significantly (P<0.05) induced an increase in Heart GPx and reduction in the Liver (P<0.01) activities while no significant effects were observed in Kidney and Erythrocyte activities when compared with the control group. Etop, in the other hand, significantly induced reduction in Kidney and elevation in erythrocyte GPx activities. The Liver and Heart GPx activities were not significantly affected by Etop administration. Co-administration of both drugs induced significant (P<0.001) reduction in the activities of Erythrocyte GPx at both intervals of administrations.
Dox treatment alone and combinations of both intervals significantly (P<0.0001) induced elevation in the synthesis of Heart GSH while no significant effect was observed when treated only with Etop (Figure 4). Also, a significant increase in the Kidney GSH was observed when animals were treated with Etop alone and at 12-h interval combination contrary to 24-h interval with significant reduction and no significant effect when expose to Dox alone. The drugs either singly or in combinations at both intervals significantly reduced Liver GSH synthesis (P<0.0001) while no significant effects were observed in an Erythrocyte GSH synthesis excerpt significant reduction at 24 h interval drug combination (P<0.01) (Figure 4).
Cardiovascular complications arising from chemotherapy are a main concern for cancer patients that are undergoing the therapy. It had been previously reported that some chemotherapeutic agents cause cardiovascular disease (CVD) through an unknown mechanism [2]. Similarly [15] and coworkers have shown that some chemotherapeutic agents perturb the normal lipid homeostasis. Meanwhile, some studies have identified lipid and lipoprotein abnormalities as an independent risk factor in the pathogenesis and progression of atherosclerosis and CVD. [16-20]. The present study, therefore, hypothesized that doxorubicin and Etoposide when administered singly or combined would lead to the perturbation of lipid dynamics and antioxidant enzyme status which are known risk factors for CVD.
A decreased plasma level of HDL cholesterol (HDL-C) observed in this study following the administration of Dox and Etop separately is a major risk factor for coronary artery disease [21]. In most cases of CVDs, lower HDL-C is secondary to hepatic elevated secretion of apolipoprotein B (apoB) containing lipoproteins [22] and hypertriglyceridemia [23]. An inadequate transport of cellular lipids to extracellular space is associated with a rapid catabolic turnover of the lipid-poor nascent HDL particles and a low HDL-C level [24]. Abnormal cellular phospholipid and cholesterol efflux has been identified as a cause of severe HDL deficiency, as seen in patients with Tangier disease (TD) and familial HDL deficiency [25]. This abnormal efflux of HDL phospholipid may have resulted in the reduction of HDL phospholipid observed in the present study. The possible consequences of a diminished HDL phospholipid, as observed in all the treated groups are reduced transport of cholesterol from atherosclerotic lesion site and thrombi to the liver, increased deposition of cholesterol at the site and reduced degradation of cholesterol in the liver. All of which makes the reduction in HDL phospholipid load a significant factor in the development of coronary artery disease. Due to the amphiphilic properties of phospholipids, their presence in HDL is an essential determinant of the capacity of the lipoprotein to remove and transport the non-polar cholesteryl esters, which contribute approximately 75% to HDL cholesterol (HDL–C). Therefore, diminished HDL–C levels are at least partly a consequence of low HDL phospholipids, as HDLs with reduced phospholipids content have been found to be poor acceptors of cell cholesterol. Correspondingly, the severity of coronary artery disease has been found to be correlated strongly with a decrease in HDL phospholipids than with an increase in HDL cholesterol [26].
Treatment with either chemotherapeutic agent, i.e. Dox or Etop triggered a hypertriglyceridemic response in the animals. Excess lipid accumulation in non-adipose tissues (lipotoxicity) may arise as a result of high plasma free fatty acids (FFAs) or triacylglycerol. It may also result from a mismatch between FFA import and utilization. Although one limitation of this study is that FFA concentration was not determined, the observed hypertriglyceridemia suggest that the two chemotherapeutic agents may be lipotoxic. Accumulation of triacylglycerol as observed in the present study is one of the risk factors of CVD, and this severe hypertriglyceridemia may be due to elevated flux of fatty acids and impaired removal of VLDL from the plasma, the latter being congruent with the elevated levels of the lipoprotein seen in the animals.
Similarly, the up-regulation of VLDL triacylglycerol concentration may be due to either increased VLDL production or decreased VLDL clearance. Meanwhile VLDL production could increase as a result of increased hepatic fatty acid synthesis, activation of adipose tissue lipolysis and suppression of fatty acid oxidation and ketogenesis. All of these aforementioned mechanisms provide more fatty acid substrate in the liver for esterification into triacylglycerol and VLDL secretion. This implies that Dox and Etop are capable of suppressing fatty acid oxidation in the mitochondria with attendant consequence on the energy yields of the lipids [27]. Meanwhile, studies have implicated hypertriglyceridemia as an early and consistent metabolic alteration during infection/ inflammation, characterized by increased VLDL triacylglycerol levels. Triacylglycerol have now been generally accepted as an independent risk factor for ischemic heart disease [28]. The concentration of triacylglycerol is thought to be mediated by the rate of synthesis of very low density lipoprotein triglyceride in the liver [29,30].
Lipoprotein lipase (LPL) is responsible for the catabolism of triacylglycerol-rich lipoprotein (VLDL) and the repression of lipoprotein E (apo-E) level [31]. A decline in its activity may contribute to a decreased clearance of VLDL, which may be responsible for the up-regulation of VLDL triacylglycerol observed in all the groups treated with the chemotherapeutic agents [32], however, noted that significant reduction in the activity of LPL is expected to have the following consequences in the lipid dynamics: hypertriglyceridemia as a result of underutilization of chylomicrons and VLDL, decreased HDL-C and HDL phospholipids as well as hypochelesterolemia. Since all these derangements were observed in the present study, it thus implies that the administration of both drugs might have the ability to down-regulate the activities of LPL.
In addition to lipotoxic and non-lipotoxic effects associated with the exposure to these chemotherapeutic agents, inhibition of paraoxonase (PON1) activity may represent another toxicodynamic. Paraoxonase is an esterase primarily synthesized in the liver and a portion secreted into the circulation, where it is associated with HDL and Apo-A1 (the structural peptide of HDL) by a lipid domain [33-35], with VLDL acting as a vector for the process [36]. PON1 is an HDL associated antioxidant enzyme that has been shown to protect the serum lipids from oxidation and can reduce macrophage foam cell formation and attenuates atherosclerosis development. Human serum PON1 activity decreases in CVD and in atherosclerotic, hypercholesterolemic, hypertensive and diabetes patients [37-39]. In this study, exposure to both doxorubicin and Etoposide individually and in combination of both intervals reduced the activities of plasma paraoxonase. Since paraoxonase is an HDL-associated enzyme and its secretion stimulated by HDL, the observed decrease in paraoxonase activity could in part, be a result of reduction in the level of HDL-C induced by doxorubicin and Etoposide when administered separately [40]. Decreased paraoxonase activity could also be accepted as an evidence of increased lipid peroxidation, since it has been shown that a decrease in paraoxonase activity is an early biochemical changes that is related to lipid peroxidation and liver injury [41-43]. The observed inhibition of paraoxonase activity could then be proposed to be through inactivation of the enzyme, a direct consequence of increased oxidative stress and inflammation [44]. Deakin and coworkers have shown that PON1 deficient mice are more susceptible to lipoprotein oxidation and atherosclerosis, while transgenic mice overexpressing PON1 display decreased atherosclerotic lesions [45]. Inhibition of PON1 by Dox and Etop as observed in this study, however, might represent an incipient biochemical event in the pathophysiology of cardiovascular damage.
Moreover, lipid metabolism dysregulation with upsurge in reactive oxygen species is a complex process and important indices for the development of cardiovascular diseases such as hypertension, infarction and coronary heart diseases [46,47]. This lipid related disease states have been shown to be linked to oxidative stress challenges in different organs [48]. A characteristic decrease and elevation of oxidative stress biomarkers are reported to be the hallmark of patients undergoing chemotherapy regimens [49]. The elevated malondialdeyde (MDA) a biomarker of lipid peroxidation in liver and heart exposed to Dox alone shows that the drugs induced significant oxido-toxicological effects on both organs. This is contrary to the effect of Etop with significant reduction in the level of kidney MDA and no significant effects on other tested organs. In addition, this study shows that Etop marred the oxidative degenerative effects of Dox when combined at different time intervals as no significant increase in MDA levels were observed in all the organs. The results of the present study are in consonant with previous reports on Dox ability to markedly increase MDA levels in heart and liver [50,51]. However, inability of Etop to induced lipid peroxidation and its protective potential against induced lipid peroxidation is consistent with the results of several studies [52,53]. This is indicative that radical produced by this drug is not strong enough to induce oxidation of membrane lipids [49] and/or Etop acts as a donor of reducing equivalents to quench radicals from initiating and propagating lipid oxidation [54].
Endogenous antioxidant enzymes such as SOD and GPx indigenously prevent free radical induced tissue damage and constituted mutually-dependent defensive mechanism against reactive oxygen species [55]. SOD catalyzes the dismutation of superoxide anion into hydrogen peroxide and molecular oxygen. It functions in conjunction with either catalase or GPx which catalyzes the toxic hydrogen peroxide to water [56]. In this study, the activities of SOD in the liver were found to be significantly decreased by both drugs either singly or in combination, contrariwise, non-significant effects were obtained in other tissues. This implies that the liver is more susceptible to the ROS induced by the two drugs. Consistent with this result is the dysregulation of GPx activities in all the tissues, either singly or in combination of the drugs. This result also shows that Dox is more virulent in the distortion of GPx activities in both the liver and heart of animals exposed to the drugs. However, combining the drugs shows significantly, increase and decrease GPx activities in the liver and erythrocyte respectively.
GSH is an ubiquitous tripeptide thiol that plays a coordinating role in the antioxidant defense mechanisms. It is known to prevent reactive oxygen species induced cellular component damage because of its reductive potential provided by the thiol group [57]. This study shows a significant increase in the levels of Heart GSH, which is likely to be related to the adaptive response to the Dox intoxication. It is also proposed to be as a result of inadequate oxidation of GSH as a part of GPx activity [58]. However, Etop treatment did not mitigate Dox- induced increase in Heart GSH levels. The increased GSH level in the heart of the animal due to Dox treatment is in agreement with previous studies [59]. Similarly, Etop treatment also induced a significant increase in the Kidney GSH contrary to the effect of Dox on the Kidney. This can also be related to the adaptive response towards the ROS induced by the Etop. Meanwhile, both drugs induced significant reduction in the status of Liver GSH levels, which consistently showing that the two drugs oxido-toxicity is more specific for the tissue.
This study shows that the lipid metabolism dysregulation relate well with the possible roles of the two drugs singly and in combinations to perpetuate pathway to cardiovascular incidence. In addition, Dox are found to substantially affect oxido-reductive balance than the Etop suggesting that the drug phenoxy radical is not strong enough to disrupt the balance.
The authors declare no competing of interest.
The authors appreciate Technical Unit of the Department of Biochemistry for their cooperation.