ISSN: 2319-9865
ISSN: 2319-9865
Department of Anatomy, Faculty of Basic Medical Sciences, Olabisi Onabanjo University, Ikenne, Ogun-State.
Received: 26/08/2012 Accepted: 14/11/2012
Visit for more related articles at Research & Reviews: Journal of Medical and Health Sciences
To determine the effect caused by the methanolic extract of Trichosanthes cucumerina seed on experimentally enlarged prostate gland in adult Wistar rats. We included 20 adult male Wistar rats, of 4 groups (Normal control NCTRL, Hormone treated control HTC, High dose of extract HDT/C, Low dose of extract LDT/C) with each group comprising of 5 animals each, with individual rats weighing between 150g-320g. The prostatic hyperplasia was achieved by the simultaneous induction of 400ng/ml of Estradiol and 1250ng/ml of Testosterone (with respect to the subject’s body weight), which were administered via the inguinal region for a period of 3 weeks (in alternate days). After the period of hormonal administration, two of the subjects from groups NC and HTC were sacrificed in other to appreciate the prostatic hyperplasia in the HTC group as compared with the NC. Furthermore, with the methanolic extract of the plant’s seed, the animals grouped in HD/TC and LDT/C was treated with respect to their body weight, for a period of 3 weeks. After which, the animals were sacrificed and the prostate glands excised for histological studies. All results were expressed as Mean ± Standard Deviation (S.D) for each group. All grouped data were statistically evaluated using SPSS 15.0 software. Hypothesis testing methods included the independent – samples t–test. Statistical significance was set at p<0.05. The experimentally induced enlargement was able to be reversed back to normal due to the effect of the methanolic extracts of Trichosanthes cucumerina seed. The combined administration of Testosterone and Estradiol caused an enlargement in the prostate due to an increase in the prostatic acini, tubules and epithelium size however there was a reversal to the normal state with the number of the prostatic acini and tubules per unit area reduced after the dosage (high and low) administration of the extract
Trichosanthes cucumerina seed, Prostate gland, Methanolic extract, benign prostatic hyperplasia, Wistar rats
Prostate Gland is a chestnut-shaped male organ, which lies between the urinary bladder and the pelvic floor surrounding the prostatic urethra. It is a compound tubuloalveoli exocrine gland of male reproductive system in most mammals [1,2]. In 2002, female parauretral glands or skene’s gland, were officially renamed the female prostate by the federative international committee on anatomical terminology [3]. A healthy adult prostate is said to be slightly larger than a walnut. Just as the prostate gland expels prostatic fluid in males during orgasm, the gland does same in the female as well [4]. The mean weight of the normal prostate in adult males is about 11grams, usually ranging between 7 and 16grams [5]. The prostate does not have a capsule rather; an integral fibromuscular band surrounds it [6] It measures about 3 cm (about 1.2 inches) across. Generally, the prostate can be divided in two ways: by zone, or by lobe. [7]. the zone classification is more often used in pathology. The idea of “zones” was first proposed by McNeal in 1968. McNeal found that the relatively homogeneous cut surface of an adult prostate in no way resembled “lobes” and thus, led to the description of “zones” [8] He has described four different regions of the prostate, the largest of the regions being the anterior fibro- muscular and non-glandular region. The remaining glandular prostate is subdivided into three zones: peripheral (PZ), central (CZ) and the traditional zones (TZ) in relation to the urethra. The peripheral zone is located posterior –laterally, the central zone is located at the base, and the 2 lobes of the transitional zone locate along the proximal urethra. The lymph vessels of the prostate drain into internal iliac lymph nodes [9].
The glandular epithelium of the prostate differentiates from theses endodermal cells, and this associated mesenchyme differentiates into dense stroma and the smooth muscle of the prostate [10]. Prostate gland represents the modified wall of the proximal portion of the male urethra and arises by the 9th week of embryonic life in the development of the reproductive system. There are histological differences between the zones e.g. in the central and peripheral glandular zones that might lead to differences in the function and presence of prostatic diseases. The ducts and acini of the peripheral and transitional zones are often smaller and not circular compared to the large ducts and acini in the central zone [9]. The prostate gland has glandular tissues and fibrous and muscular tissues around the glands. The ducts from the glands converge and open into the prostatic urethra. Individual acini have epithelium that varies from inactive, low cuboidal to active, pseudo- stratified columnar depending on the degree of stimulation by androgens. The epithelium in acini, but also in the ducts (excluding the main duct of the urethra) is composed of secretory cells that are separated from the basement membrane and prostatic stroma by a layer of basal cells. Basal cells are generally flattened, having small nuclei and only a little cytoplasm. They can be distinguished from the secretory cells, because they express specific cytokeratins and lack secretory markers. The proliferation activities of the epithelium occur in this basal cell layer. The transition epithelium, which lines the prostatic urethra and main ducts, has single layer of columnar secretory cells in the luminal surface, and only a relatively sparse cytoplasm [10].
The prostate gland produces a secretion known as prostatic fluid, which is slightly acidic, milky or whitish in appearance [11] that constitutes 20-30% of the volume of semen along with spermatozoa and seminal vesicle fluid [12]. The alkalizations of the semen is accomplished through secretion from the seminal vesicles [13]. Prostate fluid also helps to keep sperm, which is found in semen, healthy and lively, thereby increasing the chances that fertilization will occur. The prostate fluid nurtures and protects sperm during transport to potential ovum fertilization.
The prostate produces and secrets into the semen and bloodstream a 30-kDa serine prostease generally called prostate-specific antigen (PSA). The gene for PSA has two androgen response elements. PSA hydrolysis the sperm motility inhibitor semenogelin in semen, and it has several substrates in the plasma, but its precise function in circulation is unknown. Elevated plasma PSA occurs in prostate cancer and it is widely used as a screening test for this disease, though PSA is also elevated in benign prostatic hyperplasia and Prostatitis. It has a normal range between 1 and 4ng/ml.
There are three major prostate disorders; Prostatitis, Benign Prostatic Hyperplasia BPH and Prostate cancer. Prostatitis is an inflammatory condition of the prostate. There are four different forms, each with different causes and outcomes. Two relatively uncommon forms are: acute Prostatitis and chronic bacterial Prostatitis are treated with antibiotics. Chronic non-bacterial Prostatitis comprising of 95% of Prostatitis diagnosis is treated by large varieties of modalities including alpha blocker, phytotherapy, physical therapy, psychotherapy, anti-histamine and anxiolytics, nerve modulator, surgery [14] and more [15]. More recently, a combination of trigger point and psychological therapy has proved effective for category III Prostatitis as well [16]. Category IV, which is relatively uncommon in the general population, is a type of leukocytosis.
There are a variety of prostate disorders that commonly afflict men of all ages. The most common prostate disease is benign prostatic hyperplasia (BPH), a noncancerous condition of unknown cause. It occurs in approximately 70 to 80 percent of men as they reach their 70s and 80s [17]. In BPH, the prostate gland can increase in size from 20 g (0.71 oz), which is the average size of the prostate in younger men, to as large as 150 g (5.31 oz). As the prostate grows, it constricts the urethra, possibly causing a partial obstruction of the bladder. Such obstruction may lead to bladder wall thickening and urination problems. Symptoms such as frequent urination, nighttime urination, a feeling of urgency to urinate, difficulty emptying the bladder, and a weak urinary stream are the most common problems men encounter from prostate enlargement. There is evidence that it is not really uncontrolled growth of benign cells in the transition zone that is the problem, but rather a lack of controlled cell death. There are several treatment options for BPH, a minimally invasive procedure or in extreme cases, surgery that removes the prostate. Minimally invasive procedures include: transurethral needle ablation of the prostate [TUNA) and transurethral microwave therapy (TUMT) [18]. These outpatient procedures may be followed by the insertion of a temporary prostatic stent, to allow normal voluntary urination, without exacerbating irritative symptoms [19]. The surgical procedure most often used is the transurethral resection of the prostate (TURP or TUR). During this procedure, the surgeon uses an endoscope, a tube equipped with a small television camera and a sharp instrument, to cut away the excess prostate tissue [20].
Prostate cancer is one of the common cancers affecting men of older age in developed countries. And a significant cause of death for elder men [21]. Prostate cancer is treated using hormones, chemotherapy, radiation therapy, or surgical procedures
Snake gourd (Trichosanthes cucumerina) belongs to the family Cucurbitaceae mostly consumed as vegetable, but it may grow throughout the year except extreme winter. It is a popular vegetable with moderately high nutritive value. The total production of snake gourd during 2003-2004 was 136000 tons on the area of 1, 59,000 acres of land [22]. This figure indicates the low yield potentiality of our cultivars. It is commonly called as snake gourd, viper gourd, snake tomato or long tomato. The fruit is usually consumed as a vegetable due to its good nutritional value. The plant is richly constituted with a series of chemical constituents like flavonoids, carotenoids, phenolic acids which makes the plant pharmacologically and therapeutically active. Its Fruit is regarded as anthelmintic, vomitive [23] antidiabetic [24] for boil [25]. Seeds are anthelmintic, and antifebrile [26]. Root is used as purgative and tonic. The pharmacological activities of cucurbitacin containing plants have been known since ancient times. Cucurbitacins are particularly known in folk medicine for their strong purgative, anti-inflammatory, and hepatoprotective activities [27].
Adult male rats, weighing between 150g-320g were obtained from the animal house of the Department of Zoology, University of Ibadan, Nigeria. They were housed in the animal house provided by the Department of Anatomy, Olabisi Onabanjo University, where they had access to food, water, and air. Their environment was well cleaned to avoid infection of any kind upon the animals. After a week of acclimatization, the animals were induced with specific dosage of Estradiol and Testosterone (both diluted in corn oil respectively). The hormones were given based on the animal’s body weight, and the route of administration being the inguinal region. After 3weeks of induction, some of the subjects were sacrificed to appreciate the prostatic hyperplasia and their blood samples taken, to test for the prostate specific antigen. Others were then treated with the methanolic extracts of Trichosanthes cucumerina (in proportion to their body weight), diluted in corn oil. The treatment lasted for 3weeks after which the animals were sacrificed.
Drug Administration
The hormones were diluted in corn oil into 400ng/ml and 1250ng/ml of estradiol and testosterone respectively. Hormones were administered exogenously via the inguinal region for three weeks, for thrice a week in alternate days [28]. The extracts were given at 0.2mg/ml and 0.1mg/ml of high and low dosages [28]. The Testosterone was manufactured by Green Field Pharm. (JIANG SU) Co., Ltd, China while Estradiol was manufactured by Medipharm (Pvt.) Ltd., 108-Kotlakhpat Industrial Estate, Lahore
Method of Extraction
Six ripe fruits of Trichosanthes cucumerina were gotten from Ayepe, a local town in Ijebu-Remo side of Ogun State, Nigeria. The seeds were obtained from the fruit, washed in clean water; sun dried for three days, the coat peeled off, 40g of the seeds were weighed, grinded into fine powder and finally socked in 100ml of methanol. The solution was filtered after 48 hours while the filtrate was concentrated using the rotary evaporator; volume of filtrate obtained =30.6ml, weight of residue left =32g; weight of the seeds dissolved in the filtrate= 8g; volume of filtrate (oil obtained from the seeds) after evaporating = 2.5ml.
Therefore; extracts concentration = mass/volume
= 8/2.5
= 3.2g/ml
Histology
Animals were anaesthetized with chloroform in closed chamber. The thoracic vertebrate was opened under aseptic condition; the same procedure was performed throughout with paired prostates removed for histological section. The prostates were fixed in 10% formal saline, after complete fixation the blocks were embedded in paraffin and sections cut at 5 micron which was then stained with H and E and mounted in Canada balsam. Microscopic examination of the sections was then carried out under a light microscope.
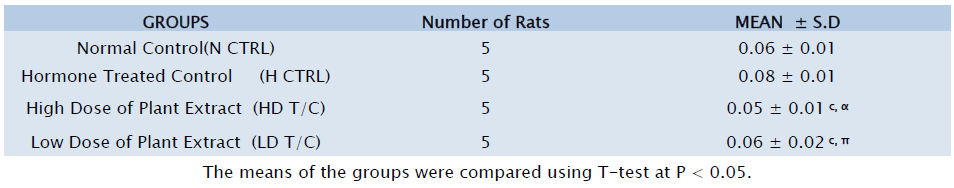
π- No significant difference between H CTRL when compared with LD T/C
c- No significant difference between N CTRL when compared with HD T/C & LD T/C
α- There is significant difference between H CTRL when compared with HD T/C
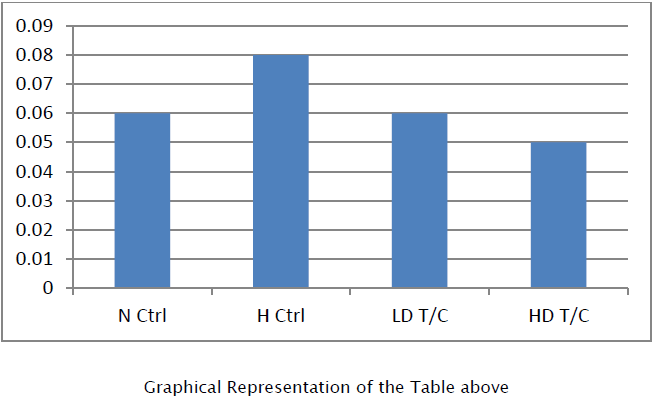
From the table, at a glance one can appreciate the anabolic effect caused by the testosterone administration [29], [30]. However, with the extracts administration, a gradual shrinkage in the prostate was observed (Prostatic atrophy), due to the withdrawal of testicular testosterone and anti-inflammatory effect of the plant [31]. Figure 1 shows the normal histological morphology of the prostate gland (prostatic concretions, excretory duct of prostate glands, glandular epithelium, smooth muscle bundles, and prostatic secretion) while in figure 2, one can notice the proliferation of the epithelial cells, the constricted follicle, a minute amount of prostatic concretion and little or no prostatic secretion. All these can be attributed to the anabolic hormonal effect of the testosterone and estradiol. In addition, figure 3 shows an approach towards the reversal to the initial histological morphology of the prostate. Finally, in figure 4, one can appreciate the anti-inflammatory effect haven accomplished by the extract as the prostate tissue seems to approach the initial histological morphology. The epidemiology of BPH is complex and not fully understood. The androgenic hormones testosterone and dihydrotestosterone play at least a permissive and important role. Growth factors and other hormones including estrogens may also play a role. BPH is a truly hyperplasic process resulting in growth of glandular epithelial and stromal/muscular tissues in the prostate, leading to often measurable growth taking on different shapes and configuration which may impact symptoms and secondary outcomes [32].
After the period of high dose administration, there was a decrease in weight of the prostates. The weight loss may be attributed to the degradation of basement membrane and interstitial tissues and absence of cell proliferation due to depletion of androgens in the animals. Administration of androgens; Testosterone (T) and Estradiol (E) induced increases in the prostate weights in the rats and that may be due to cell proliferation and stromal growth [32]. The stroma provides the infrastructure for the development of epithelial cells, the results confirms the anabolic effects of androgens reported by Adesanya e.al., [28]. Complex interactions between androgen and estrogen regulate prostatic growth, development and physiology. The hypertrophy of the epithelial cells suggests that addition of E potentiates the action of T, causing an increase in the thickness of epithelial cells which can directly stimulate the activity of secretory epithelial cells.
This study provides a model for demonstrating the mechanism of prostatic enlargement in the aging prostate. It suggests that there is some level of conversion of Testosterone to estradiol-17-beta in the aging prostate by the enzyme aromatase and the estrogen so produced though at low level synergizes the effect of T and its metabolite dihydrotestosterone DHT in the prostate thereby leading to prostatic hypertrophy however such effect can be reversed by the administration of methanolic extract of Trichosanthes cucumerina seed due its anti-inflammation effect on the prostate [31].
The combined administration of Testosterone and Estradiol caused an enlargement in the prostate due to an increase in the prostatic acini, tubules and epithelium size however there was a reversal to the normal state with the number of the prostatic acini and tubules per unit area reduced after the dosage (high and low) administration of the extract.
T/C- Trichosanthis cucumerina, METC- Methanolic extract of Trichosanthes cucumurina seed, MEAN ± SD- Mean plus OR minus Standard Deviation, p<0.05- Statistical significance was set at p< 0.05, t-test- samples t–test
I wish to express my sincere gratitude to the co-authors as well as the technical staff of the Anatomy Department OOU, Ikenne Ogun-State Nigeria, for their support in execution of this work.