e-ISSN: 2320-7949 and p-ISSN: 2322-0090
e-ISSN: 2320-7949 and p-ISSN: 2322-0090
1Department of Oral Medicine and Radiology, Madha Dental College and Hospital, Madha Nagar, Somangalam Road, Kundrathur, Chennai - 600 069,Tamilnadu, India.
2Department of Periodontics, Madha Dental College and Hospital, Madha Nagar, Somangalam Road, Kundrathur, Chennai - 600 069,Tamilnadu, India.
Received: 15/05/2014 Revised: 18/06/2014 Accepted: 23/06/2014
Visit for more related articles at Research & Reviews: Journal of Dental Sciences
Erythema multiforme is a rare acute inflammatory disorder involving skin and mucous membrane.It can clinically be minor or major form or involve only oral mucosa.Various agents have been reported to trigger erythema multiforme.Here we report a unusual case of erythema multiforme which is caused by drug involving the oral mucosa and have discussed how important it is to differentiate other ulcerative lesions of oral cavity from erythema multiforme As oral physicians we will be the first to encounter such cases,so we also emphasize on its early diagnosis and appropriate management.
Erythema multiforme, antibiotics, mucocutaneous disease, steroids
Erythema multiforme(EM) is an uncommon, typically mild self-limiting, acute inflammatory disorder which affects the skin and/or mucous membranes[1,2]. EM usually affects healthy young adults and reports suggest that males are more affected than females. Peak age at presentation is between 20-40 years, although 20 % cases are children1.
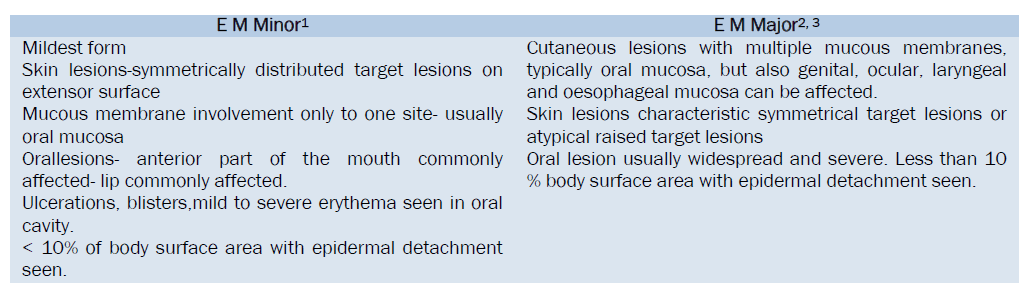
Based on the severity and the number of mucosal sites involved, disease has been subclassified into EM minor and major [3]. Few reports have stated about oral EM as a third variant of EM[4]. EM involving only oral mucosa is a separate entity or is a part of minor form of EM is unclear[5]. Oral EM, even though may be confined only to oral mucosa, may later manifest severe forms of EM with involvement of skin and mucosa. EM has been reported to be triggered by numerous agents, particularly virus, and a variety of other infectious agents, food additives, chemicals and drugs [1].
Oral cavity is an important source of diagnostic information.6Patients presenting with oral EM without any cutaneous involvement will primarily visit a dentist, so it is important to identify and distinguish the disorders for early management and proper follow up. Here we present a case of oral erythema multiforme in a 43 year old female patient which was triggered due to intake of drugs.
Case Report
A 43 year old female patient reported to our dental OP with complaints of pain and ulceration in the lip since four days. Patient gave a history of sudden onset of ulceration and bleeding from the ulcers and had difficulty in eating and swallowing. There was history of fever and sore throat one week back when the patient had visited a general physician, and patient gave a positive drug history of having taken cephalosporin. Following the intake of drugs, she developed multiple bullae and small ulcers in the lips which later transformed into extensive, large bleeding ulcers.(Figure 1) Patient did not have any systemic illness and all the vitals were normal.On clinical examination, the lips were swollen and cracked; there were large ulcers in the upper and lower lip with irregular borders. There were also haemorrhagic encrustations over the ulcer. Some ulcers were bleeding on provocation. (Figure 2) The submandibular lymph nodes were palpable bilaterally and were tender and soft in consistency.
Intra oral examination reveals bleeding ulcers in the buccal mucosa, labial mucosa, mainly in the anterior part of oral cavity.(Figure 3) The ulcers were extensive with sloughing and erythematous borders. There was no other lesion anywhere else in the body. A positive drug history, sudden onset, extensive ulcerations with bleeding and crustations over the ulcer strongly lead to a diagnosis of erythema multiforme. The patient was first advised to stop the intake of cephalosporins and the patient was treated with prednisolone 10mg thrice daily for one week, then twice daily for the second week and slowly tapered to once daily in the third week. Also, topical clobetasoldipropionate 0.05 % was given with topical application of lignocaine gel to facilitate fluid intake. The patient was reviewed after four days and the condition was noticed to have significantly improved,(Figure 4,5,6) and then again after ten days which showed total resolution of the ulcers without any scarring.( Figure 7,8) The patient was also advised not to take any drug from the cephalosporin group. The patient was under regular follow ups for the next one year with no evidence of any recurrence.
EM is an acute self-limiting, sometimes recurrent hypersensitivity reaction [7]. It affects skin or oral mucous membrane or both[8]. EM can be induced by adverse drug reaction with a frequency of more than 1 %[9]. Drugs such as sulfonamides, cephalosporins, amino penicillins, quinolones, chlormezanone, barbiturates, oxicamnon-steroidalanti-inflammatory drugs, anti convulsants, allopurinol or even corticosteroids may be implicated. Other etiological factors include viruses, other infectious agents, food additives and chemicals. The exact pathogenesis is unknown, but it is suggested that EM results from T cell mediated immune reaction to the precipitating agent which leads to a cytotoxic attack on keratinocytes that express non-self-antigens leading to sub epithelial and intraepithelial vesciculation[10].
The clinical presentation of EM ranges from a self-limited, mild exanthematous variant with minimal oral involvement to a severe widespread and life threatening illness[2,10]. The skin lesions are classified as typical target lesions which are usually symmetrical and consist of macules or papules with or without blisters. Skin lesions are accompanied by ulcerations of the mucous membrane, particularly oral mucosa. Also other mucosa like eye and genital can also be involved.
Originally the disease was classified as either EM minor or major and distinction between the two depended principally on the extent of mucosal involvement.
Oral lesion usually widespread and severe. Less than 10 % body surface area with epidermal detachment seen.
In Steven Johnson’s syndrome, there is atypical flat target lesions and macules rather than classic target lesions. There are also systemic symptoms. Generally widespread rather than involving only acral areas. Multiple mucosal sited with scarring of mucosal lesions. About less than10% body surface area with epidermal detachment seen.
Toxic epidermal necrolysis (TEN) has no typical target, flat atypical targets with severe mucosal erosions and progress to diffuse generalized detachment of epidermis. The body surface with epidermal detachment is greater than 10 %[11].
Many authors have suggested the new category of EM affecting the oral cavity, which is oral EM without any skin lesions[3]. Oral EM is a chronically recurrent condition with frequency of episodes varying from every three weeks to once yearly. But our case did not report of any recurrence on regular follow up for one year. With the clinical appearance seen in our case and also a positive relationship between the drug intake and occurrence of the oral mucosal lesions, it was diagnosed as oral EM. Also, our case started a few days after the drug intake and completely resolved after the cessation of the drug. This was also a strong reason for diagnosis.
The differential diagnosis given to our case were lesions pertaining to the oral cavity like herpes, vesciculobullous lesions such as pemphigus vulgaris, bullous pemphigoid and other drug reactions. Herpetic lesions were ruled out because of the location, keratinized mucosa and absence of any gingival ulceration. A positive drug history associated with the onset of ulcerations in our case ruled out autoimmune vesciculobullous lesions.3 Bullous lichen planus may also show similar lesions, but absence of Wickham’s striae in our case excluded its diagnosis.12 Other drug reactions include mucosal fixed drug eruptions, lichenoid drug reaction, pemphigoid like drug eruptions, which all were excluded depending upon the clinical appearance in our case[3].
There is no specific diagnostic test for EM and is mainly clinically supported.biopsy of perilesional tissue with histological and immunostainingexamination is essential if a specific diagnosis is required.immunostaining shows intense lymphocytic infiltration at the basement membrane zone and perivascularlynon-specific immune depositsif IgM, C3 and fibrin at these sights[10].The treatment of EM is non-specific, but supportive care is important. The causative drug agent should be identified and withdrawn.9Also supportive care like topical analgesics, topical anesthetics, sootheniing mouth rinses, bland diet can be given[11,13]. If any herpes virus is identified, then antiviral agents are indicated. Acyclovir 200mg can be given five times daily, or 400 mg four times daily or valacyclovir 500mg twice a day can be given for five days[10]. Also, systemic steroids can be given. Prednisone in doses upto 1mg/kg daily, tapered over 2-3 weeks[3]. Also, immunosuppressive drugs like dapsone, azathioprine, mycophenolate, and cyclosporine can be given[12]. Steven Johnson syndrome patients are treated in burn units with porcine xenografts.
Since erythema multiforme has no appropriate diagnostic test, the early recognition and diagnosis of the disease plays a very vital role. Thus, as oral physicians, we might be the first to encounter such diseases, and a quick diagnosis, withdrawal of the causative agent and prevention of the recurrence of the disease becomes our important role.